Scientists from Stanford University found that a common antidepressant, fluoxetine (commonly known as Prozac), appears to target glioblastoma.
Further, real-world data from electronic medical records suggests that glioblastoma patients prescribed Prozac along with the standard treatment for the disease survived longer.
The research is published in Cell Reports and was conducted by pathologist Paul Mischel et al.
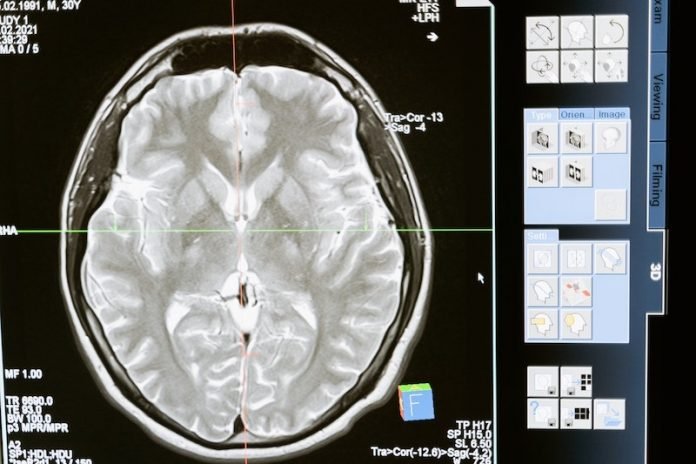
Glioblastoma is a difficult to treat, often deadly, brain cancer.
It’s the most common malignant brain cancer in adults, but scientists don’t have any way to detect it early, and treatments are often ineffective.
The brain’s unique makeup is part of what makes these cancers difficult to treat.
It’s sequestered from the rest of the body by the blood-brain barrier, which protects precious nerve cells from potential bad agents circulating in the bloodstream.
But this barrier also prohibits the entry of many medications—another hurdle to overcome when designing drugs to target brain cancers.
Finally, glioblastomas are known to have many copies of cancer-associated genes, including one called the epidermal growth factor receptor, or EGFR.
The team knew that the balance of cholesterol and a class of fats called lipids is often severely disrupted in glioblastoma cells. They also knew that these lipids are important in EGFR signaling.
After a series of deductions, they homed in on a lipid called sphingolipid as potentially important in glioblastoma growth and survival.
They found that people with glioblastomas whose cancers made high levels of an enzyme involved in sphingolipid metabolism called SMPD1 had much shorter lifespans than patients whose cancers expressed lower levels of the enzyme.
The team next searched the scientific literature for compounds that can inhibit SMPD1 and also cross the blood-brain barrier.
They found that fluoxetine, or Prozac, achieves both of these goals. It’s known to be safe, it can enter the brain, and it can inhibit SMPD1.
And when the team gave Prozac at a safe dose to mice with human glioblastomas, the levels of the EFGR oncogene went down strongly and the tumors melted away and didn’t come back.
Because fluoxetine is widely used as an antidepressant, the team wondered whether any evidence existed for an effect on glioblastoma.
So they surveyed the electronic medical records of a large insurance claims database to identify people with glioblastomas who had also been taking fluoxetine during their illnesses.
They found that patients who had received Prozac, along with the standard of care for glioblastomas, lived much longer than the control group.
The researchers plan to partner with the National Brain Tumor Society to design a clinical trial to test the effect of fluoxetine in people with glioblastomas.
Sign up for our newsletter for more information about this topic.
If you care about brain health, please read studies about how sleep affects human brain clearance, and vitamin B may prevent brain loss.
For more information about brain health, please see recent studies about iron in the brain linked to cognitive decline, and results showing smoking harms your brain health, regardless of other health conditions.
Copyright © 2022 Knowridge Science Report. All rights reserved.




