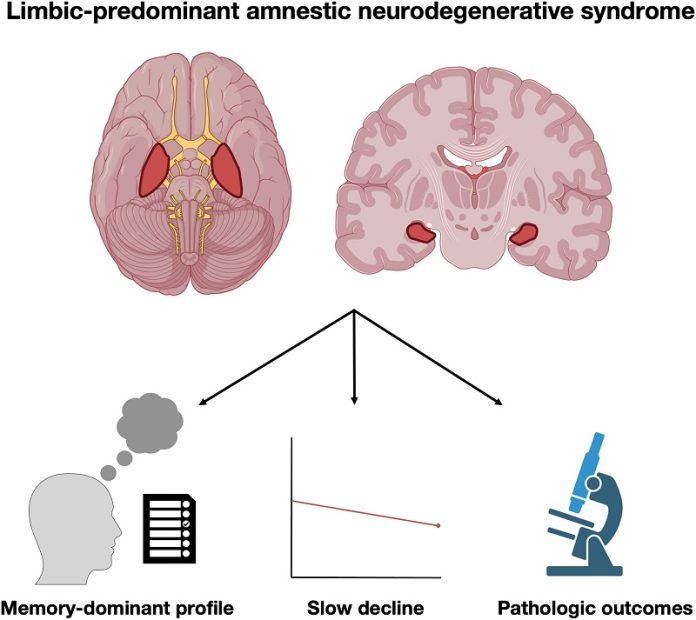
Researchers at the Mayo Clinic have discovered a new type of memory loss syndrome in older adults that affects the brain’s limbic system.
This syndrome, named Limbic-predominant Amnestic Neurodegenerative Syndrome (LANS), can often be mistaken for Alzheimer’s disease.
The good news is that LANS progresses more slowly and has a better prognosis than Alzheimer’s.
Before this discovery, doctors could only confirm LANS by examining brain tissue after a person’s death.
Now, thanks to the new criteria published in the journal Brain Communications, doctors can diagnose LANS in living patients.
This framework helps neurologists and other experts to classify the condition more accurately, leading to better treatment options.
The criteria consider several factors, including age, the severity of memory impairment, brain scans, and biomarkers indicating the presence of specific proteins in the brain. These criteria were developed and validated using data from more than 200 participants in various studies, including the Mayo Clinic Alzheimer’s Disease Research Center and the Alzheimer’s Disease Neuroimaging Initiative.
Understanding LANS will help doctors manage symptoms more effectively and offer more tailored therapies for patients. Dr. David T. Jones, a Mayo Clinic neurologist and senior author of the study, explains that this new framework allows doctors to provide more precise diagnoses.
“In our clinical work, we see patients whose memory symptoms appear to mimic Alzheimer’s disease, but their brain imaging or biomarkers show they don’t have Alzheimer’s.
Until now, there has not been a specific medical diagnosis to point to, but now we can offer them some answers,” he says.
This research has significant implications for treatment decisions, including the use of amyloid-lowering drugs and participation in new clinical trials. It also helps in counseling patients about their prognosis, genetics, and other factors.
Nick Corriveau-Lecavalier, the study’s first author, highlights that decades of work have gone into understanding and classifying different types of dementia. These findings build on ongoing efforts to untangle neurological conditions that have similar symptoms but different treatments and outcomes.
“Historically, you might see someone in their 80s with memory problems and think they have Alzheimer’s disease. With this paper, we are describing a different syndrome that happens much later in life. Often, the symptoms are restricted to memory and will not progress to impact other cognitive areas, so the prognosis is better than with Alzheimer’s disease,” he explains.
Researchers also looked at the involvement of a protein called TDP-43, which they found in the brain tissue of older adults who had passed away. This protein buildup, known as limbic-predominant age-related TDP-43 encephalopathy (LATE), might be linked to LANS, but further research is needed.
With the new clinical criteria established by Dr. Jones, Corriveau-Lecavalier, and their co-authors, doctors can soon diagnose LANS in patients, helping those living with memory loss to better understand their treatment options and the potential progression of their condition.
This opens the door for more research to further clarify the characteristics of this newly defined syndrome.
If you care about dementia, please read studies about low choline intake linked to higher dementia risk, and how eating nuts can affect your cognitive ability.
For more information about brain health, please see recent studies that blueberry supplements may prevent cognitive decline, and results showing higher magnesium intake could help benefit brain health.



