A groundbreaking study by researchers at Pohang University of Science and Technology (POSTECH) has identified a key protein that promotes the development of systemic lupus erythematosus (SLE), a common autoimmune disease.
The research team, led by Professor Yoontae Lee and Ph.D. candidate Jiho Park, published their findings in the journal, Proceedings of the National Academy of Sciences (PNAS).
SLE is a complex autoimmune disease that often presents with a butterfly-shaped red rash on the face and arthritis.
It primarily affects the nose and cheeks, but its symptoms and the immune cells involved can vary greatly between patients.
This variability has made it challenging to understand the disease fully and to develop effective personalized treatments.
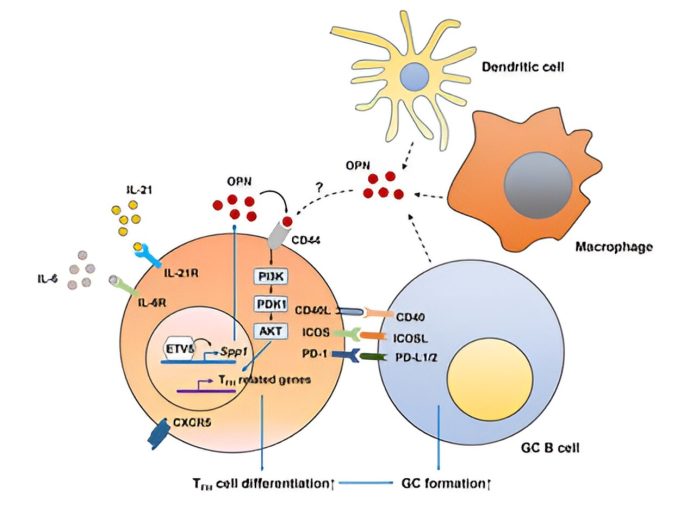
The immune system is our body’s defense mechanism, with B cells playing a crucial role by producing antibodies to fight off invaders like viruses. T follicular helper (TFH) cells support B cells in this process.
However, an excess of TFH cells can cause B cells to become overly active. This hyperactivity can lead to autoimmune diseases where B cells mistakenly attack the body’s own tissues, thinking they are harmful pathogens.
Previous research by Professor Lee’s team indicated that a transcription factor called ETV5, found in T cells, could be responsible for pushing T cells to become TFH cells, potentially triggering SLE.
In their latest study, the team conducted experiments on mice and humans to test this theory.
The results were promising. In mice models lacking ETV5, symptoms of autoimmune diseases such as high levels of autoantibodies, infiltration of immune cells into body tissues, and kidney inflammation were significantly reduced. The development of TFH cells also decreased. This suggested that ETV5 played a critical role in the disease.
Further investigation revealed that ETV5 boosts the production of a protein called osteopontin (OPN), which then activates another protein, AKT, leading to the creation of more TFH cells. The researchers also confirmed that the same process happens in human T cells.
In patients with SLE, levels of ETV5 and OPN were found to be higher compared to healthy individuals. Moreover, the severity of the disease and the concentration of autoantibodies in the blood were linked to the levels of ETV5 and OPN.
Professor Yoontae Lee stated, “We have identified a mechanism of SLE pathogenesis involving ETV5 and OPN in real-world experiments. We hope that further research will lead to the development of ETV5 inhibitors that regulate TFH cell development to help treat SLE patients.”
This discovery brings new hope for better understanding and treating SLE, potentially paving the way for new therapies that target ETV5 and OPN to manage this challenging autoimmune disease effectively.
If you care about health, please read studies about how Mediterranean diet could protect your brain health, and the best time to take vitamins to prevent heart disease.
For more health information, please see recent studies that olive oil may help you live longer, and vitamin D could help lower the risk of autoimmune diseases.



