New research from the University of Kentucky’s Sanders-Brown Center on Aging has revealed that the cognitive impairments seen in long COVID patients are strikingly similar to those observed in Alzheimer’s disease and related dementias.
This discovery could open new doors for understanding and treating these brain disorders.
The study, published in Alzheimer’s & Dementia, involved a global team of experts in neuroscience, led by researchers at the UK College of Medicine.
Key contributors included Dr. Yang Jiang, a professor in the Department of Behavioral Science, Dr. Chris Norris, a professor in the Department of Pharmacology and Nutritional Sciences, and Dr. Bob Sompol, an assistant professor in the same department.
Their research focused on brain functions, inflammation, and the role of support cells in the brain known as astrocytes.
“This project benefited greatly from interdisciplinary collaboration,” said Dr. Jiang. The study involved contributions from scientists across six countries, including the U.S., Turkey, Ireland, Italy, Argentina, and Chile.
The research focused on the “brain fog” that many COVID-19 survivors experience, even months after recovering from the virus. Symptoms of brain fog include memory problems, confusion, and difficulty concentrating.
Dr. Jiang explained, “The slowing and abnormality of brain activity in COVID-19 patients resemble those seen in Alzheimer’s and related dementias.”
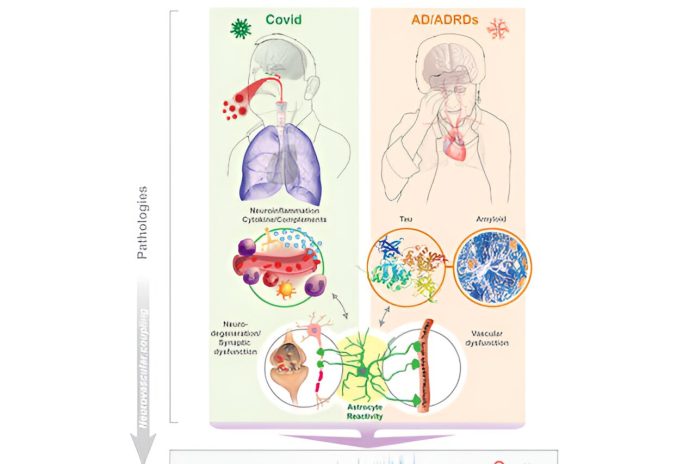
The study suggests that long COVID and Alzheimer’s disease may share similar biological processes. Both conditions involve brain inflammation, the activation of astrocytes, and abnormal brain activity, leading to significant cognitive impairments.
“The idea that COVID-19 could lead to Alzheimer’s-like brain changes is a significant development,” Dr. Jiang noted. “People don’t usually connect COVID-19 with Alzheimer’s disease, but our review of emerging evidence suggests otherwise.”
One of the most important findings is the role of astrocytes, which are brain support cells that have not been as thoroughly studied as neurons. The research suggests that COVID-19 can damage or activate these cells, leading to synaptic dysfunctions and abnormal brain activity similar to that seen in early neurodegenerative diseases like Alzheimer’s.
The study also emphasizes the importance of regular brain function check-ups for COVID-19 survivors, particularly using affordable tools like electroencephalography (EEG).
EEG patterns in COVID-19 patients have been found to resemble those seen in early stages of neurodegenerative diseases. This similarity could be due to shared issues such as brain inflammation, astrocyte activity, low oxygen levels, and blood vessel damage.
The researchers believe that routine EEG exams could help detect early brain changes in COVID-19 survivors, potentially allowing health care providers to identify at-risk individuals sooner and implement interventions to prevent or slow cognitive decline.
As the research continues, the team is particularly interested in how EEG monitoring can predict long-term outcomes in COVID-19 patients and assess the effectiveness of treatments aimed at preventing cognitive decline.
This work could have a significant impact on patient care, providing new strategies for addressing cognitive issues related to both COVID-19 and neurodegenerative diseases like Alzheimer’s.
If you care about Alzheimer’s disease, please read studies about vitamin D deficiency linked to Alzheimer’s and dementia, and strawberries can be good defence against Alzheimer’s.
For more health information, please see recent studies about foods that reduce Alzheimer’s risk, and oral cannabis extract may help reduce Alzheimer’s symptoms.
Source: University of Kentucky.



