Researchers at UC San Francisco have developed a groundbreaking approach to treating Parkinson’s disease with a new type of brain implant called adaptive deep brain stimulation (aDBS).
This technology promises personalized, round-the-clock care for people with Parkinson’s, adjusting to their needs throughout the day and even helping with sleep at night.
Parkinson’s disease affects about 10 million people worldwide. It occurs when dopamine-producing neurons in the brain, which control movement, die off.
This loss of dopamine leads to symptoms like tremors, stiffness, and uncontrolled movements.
Traditional treatments include the drug levodopa, which replaces dopamine.
However, this drug can cause side effects, such as uncontrolled movements (dyskinesia) when dopamine levels are too high and a return of stiffness when the drug wears off.
To manage these symptoms, some patients receive a constant deep brain stimulation (cDBS) device, which provides steady electrical stimulation to the brain.
While cDBS can reduce the need for medication and help control symptoms, it isn’t perfect.
It can sometimes overstimulate or understimulate the brain, leading to swings in symptoms throughout the day.
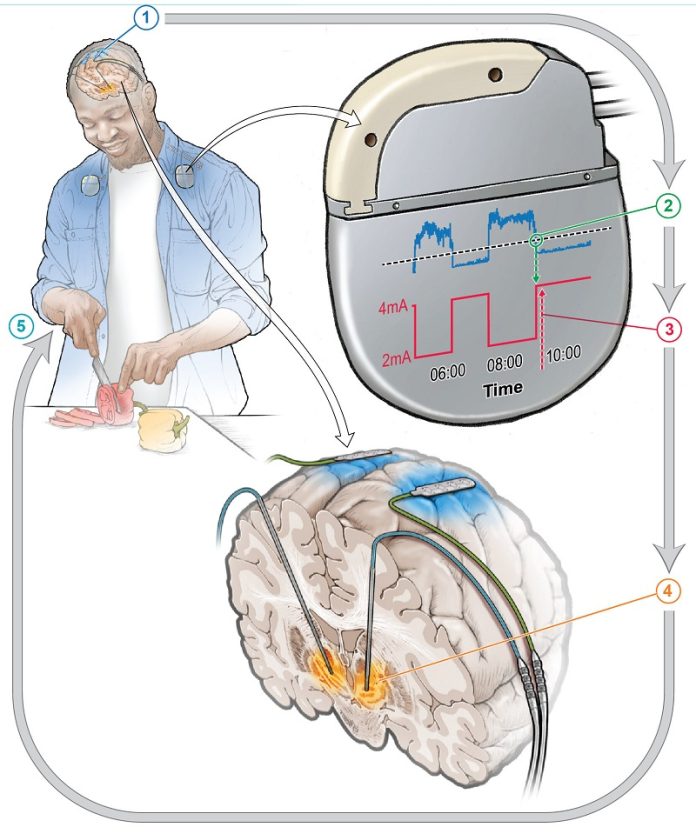
The new aDBS system is different. It uses artificial intelligence to monitor brain activity in real time and adjusts the stimulation levels based on the patient’s needs at any given moment.
This “closed-loop” system creates a continuous feedback loop, where the device reads brain signals and responds instantly, providing just the right amount of stimulation.
In a clinical trial, researchers tested the aDBS system on four patients, comparing it to the traditional cDBS device.
The patients were asked to identify their most bothersome symptom, and the aDBS technology reduced these symptoms by 50%. The results of this study were published in Nature Medicine.
“This is the future of deep brain stimulation for Parkinson’s disease,” said Dr. Philip Starr, co-director of the UCSF Movement Disorders and Neuromodulation Clinic and one of the study’s senior authors. Dr. Starr has been working on this technology for over a decade, developing ways to detect abnormal brain rhythms associated with Parkinson’s and identifying specific patterns linked to motor symptoms.
Earlier this year, another study led by UCSF researchers showed that aDBS could also help with insomnia, a common problem for Parkinson’s patients. This is significant because traditional DBS devices primarily focus on daytime movement symptoms and don’t address sleep issues.
In this study, the aDBS device was able to detect brain activity related to different sleep states and even predict when a patient was likely to wake up during the night.
These findings were published in Nature Communications.
The aDBS system works by recognizing brain signals in the motor cortex, a region of the brain that controls movement.
This is different from the cDBS approach, which targets the subthalamic nucleus (STN), another brain area involved in movement coordination. The motor cortex signals are less likely to be disrupted by the stimulation, making them more reliable for controlling the aDBS device.
The researchers also developed personalized algorithms for each patient, allowing the aDBS system to respond to the unique brain activity associated with their symptoms. This approach could lead to more precise and effective treatments, not only for Parkinson’s but also for other neurological disorders like depression and obsessive-compulsive disorder (OCD).
The work is part of a larger effort to develop “smart” neurostimulation therapies that can adapt to a patient’s needs in real time.
According to Dr. John Ngai, director of the NIH’s Brain Research Initiative, “This personalized, adaptive DBS embodies the mission to revolutionize our understanding of the human brain.”
As scientists continue to refine this technology, the potential impact on patients’ lives could be profound.
“We’re at the beginning of a new era of neurostimulation therapies,” said Dr. Starr. The aDBS system not only offers hope for better management of Parkinson’s disease but also opens the door to treating a wide range of neurological conditions more effectively.
If you care about brain health, please read studies that eating apples and tea could keep dementia at bay, and Olive oil: a daily dose for better brain health.
For more health information, please see recent studies what you eat together may affect your dementia risk, and time-restricted eating: a simple way to fight aging and cancer.



