A recent study by Ludwig Cancer Research has uncovered a crucial metabolic switch in the immune system’s T cells that plays a vital role in creating long-lasting immunity and enhancing the body’s ability to fight tumors during cancer immunotherapy.
The research, led by Ping-Chih Ho and Alessio Bevilacqua from Ludwig Lausanne, was published in Science Immunology and sheds light on how this switch, known as PPARβ/δ, helps T cells become powerful defenders against both infections and cancer.
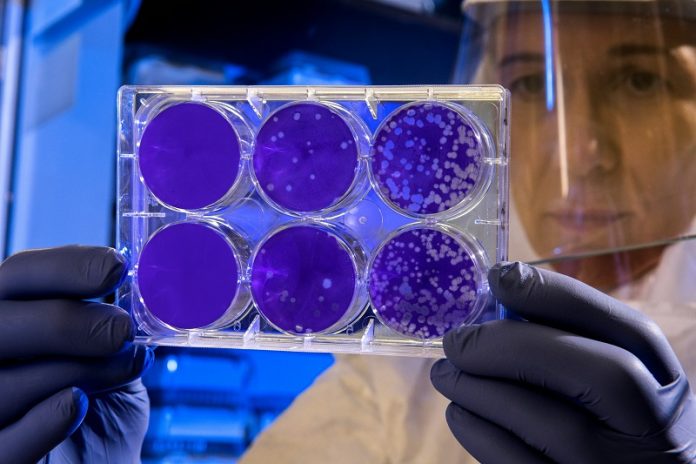
T cells, particularly a type called CD8+ T cells or “killer” T cells, are essential for eliminating infected or cancerous cells.
When these T cells encounter a threat, they activate specific metabolic pathways to fuel their rapid growth and attack.
However, after the threat is neutralized, most of these T cells die off. A small number, however, transform into central memory T cells (Tcms) that remain in the body, ready to respond quickly if the same threat reappears.
Until now, scientists didn’t fully understand how this transformation occurs.
The Ludwig research team discovered that PPARβ/δ, a master regulator of gene expression, is the key to this process.
By activating this switch, T cells can shift their metabolism to survive over the long term, becoming memory T cells that patrol the body and provide lasting immunity.
The study found that when the PPARβ/δ switch is disrupted, T cells struggle to make this important transformation, leading to a weakened immune memory.
This discovery is particularly significant because it could lead to new ways of improving cancer immunotherapy—a treatment that helps the immune system fight cancer more effectively.
One of the study’s major findings is that PPARβ/δ is not only crucial for memory T cells but also plays a vital role in a specific type of T cell found in tumors.
These cells, called progenitor-exhausted T cells, can either become “terminally exhausted” and ineffective or, with the right stimulus, turn into “effector” T cells that actively attack and kill cancer cells.
The researchers showed that PPARβ/δ helps prevent these T cells from becoming exhausted, keeping them ready to fight cancer.
To test the potential of targeting PPARβ/δ in cancer treatment, the researchers exposed T cells to a molecule that activates this switch and then used these treated cells in a mouse model of melanoma, a type of skin cancer.
The treated T cells were more effective at slowing tumor growth compared to untreated cells, showing that activating PPARβ/δ could be a promising strategy in cancer therapy.
“Our findings suggest that targeting PPARβ/δ could enhance the effectiveness of T cell-based cancer treatments,” said Bevilacqua. “This approach might help keep T cells in a state where they can better fight tumors.”
While this research is still in its early stages, the discovery of PPARβ/δ’s role in T cell function opens up exciting possibilities for new cancer therapies.
Further studies are needed to determine how best to target this switch in humans, but the potential to boost the body’s natural defenses against cancer is a promising avenue for future research.
If you care about cancer, please read studies about vitamin D and bowel cancer, and a cautionary note about peanuts and cancer.
For more health information, please see recent studies about the link between ultra-processed foods and cancer, and everyday foods to ward off pancreatic cancer.



