A new study led by Washington University School of Medicine in St. Louis has found that the risk of developing long COVID has decreased significantly throughout the pandemic.
Researchers credit 70% of this reduction to COVID-19 vaccinations and 30% to changes in the virus and improved detection and management methods.
Published in The New England Journal of Medicine, the study highlights the positive impact of vaccinations on long COVID.
“This is a rare occasion where I have good news to report about this virus,” said Dr. Ziyad Al-Aly, senior author and a leading expert in COVID-19 research. “The findings show the positive effects of getting vaccinated.”
Long COVID refers to lingering and debilitating health effects experienced by about 10% of people who have had COVID-19. Since the pandemic began, over 775 million cases of COVID-19 have been documented by the World Health Organization.
Dr. Al-Aly has extensively studied the virus’s long-term impacts on various organ systems, including the heart, brain, kidneys, and gastrointestinal (GI) tract. Despite the reassuring findings of this study, he emphasized that long COVID is still a concern. “We cannot let our guard down,” he said. “Annual COVID vaccinations are key to reducing long COVID risk. If we stop vaccinations, the risk is likely to increase.”
Dr. Al-Aly and his team analyzed millions of de-identified medical records from the U.S. Department of Veterans Affairs, covering 441,583 veterans with COVID-19 and over 4.7 million uninfected veterans from March 1, 2020, to January 31, 2022. The study included people of diverse ages, races, and sexes to ensure fair representation.
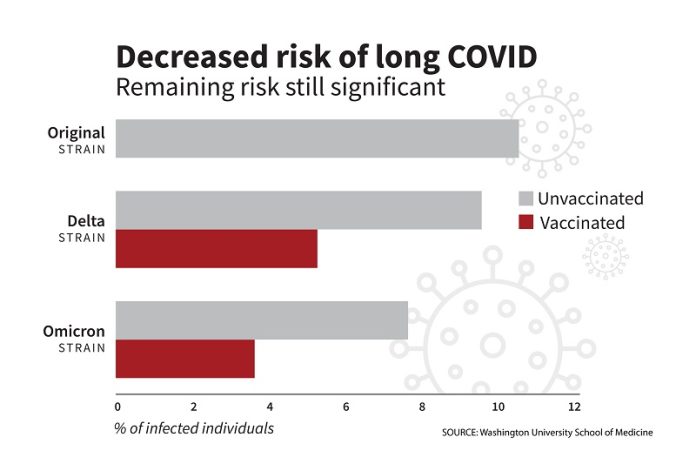
The researchers divided the veterans into five groups: unvaccinated individuals with the original COVID-19 strain (2020), the delta variant (2021), and the omicron variant (2022); and vaccinated individuals with the delta and omicron variants. They then estimated the rates of long COVID one year after infection for each group.
The highest rate of long COVID was seen in those infected with the original strain, with 10.4% developing long-term symptoms. This rate dropped to 9.5% during the delta variant era and 7.7% during the omicron variant era for unvaccinated individuals. Among vaccinated individuals, the rate was 5.3% during the delta era and 3.5% during the omicron era.
“There is a clear difference in risk between vaccinated and unvaccinated individuals during the delta and omicron eras,” Dr. Al-Aly said. “Deciding to forgo vaccinations essentially doubles the risk of developing long COVID.”
Even with the overall decline, the lowest rate—3.5%—is still significant. “That’s three to four vaccinated individuals out of 100 getting long COVID,” Dr. Al-Aly explained. “With many people still getting infected, this remaining risk is substantial.”
Dr. Al-Aly also noted that each COVID-19 variant affects different parts of the body. While the original virus targeted the respiratory system, the omicron variant was more associated with metabolic and GI issues. “It’s important to understand these differences as they impact long COVID risk and treatment.”
While the decline in long COVID risk is good news, Dr. Al-Aly stressed the need for continued research to prevent and treat long COVID, as millions of people are still affected.
If you care about COVID-19, please read studies about vitamin D deficiency linked to severe COVID-19, death, and how diets could help manage post-COVID syndrome.
For more information about COVID, please see recent studies that low-sodium plant-based diets may prevent COVID-19 better, and results showing zinc could help reduce COVID-19 infection risk.
Source: Washington University School of Medicine.



