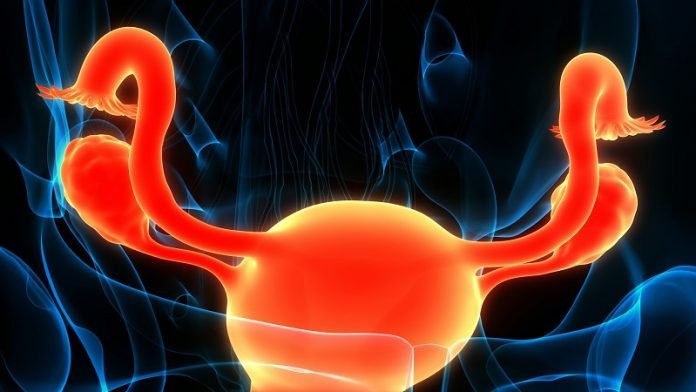
The ovaries, part of the female reproductive system, are akin to tiny but mighty engines driving the production of eggs and hormones.
However, like any complex system, things can go awry, leading to conditions such as ovarian cysts and, more seriously, ovarian cancer.
While these conditions may seem linked by their location, their relationship is nuanced, and understanding the connection—or lack thereof—between them can empower women with knowledge about their reproductive health.
Ovarian cysts are fluid-filled sacs on the ovary and are incredibly common. They’re often a normal part of the menstrual cycle, known as functional cysts, which usually resolve on their own without treatment. These cysts are benign, meaning they’re not cancerous.
However, there are also pathological cysts, which are less common and may be benign or malignant (cancerous). These can include dermoid cysts, cystadenomas, and endometriomas, each with unique characteristics but not necessarily indicative of ovarian cancer.
On the other hand, ovarian cancer refers to malignant growths that arise from different tissues within the ovary. It’s known as a “silent” disease because its symptoms are incredibly subtle in the early stages, often going unnoticed until the cancer has advanced.
Symptoms can include bloating, pelvic pain, abdominal swelling, and urinary urgency, which can easily be mistaken for other benign conditions, including ovarian cysts.
The link between ovarian cysts and ovarian cancer is a topic of ongoing research and discussion. Most ovarian cysts are benign and don’t increase the risk of ovarian cancer.
However, certain types of cysts and complex cysts with solid areas, septations, or nodules may require closer monitoring for potential malignancy.
The risk factors for developing ovarian cancer include genetics (such as mutations in the BRCA1 or BRCA2 genes), family history of ovarian or breast cancer, age, and reproductive history, among others.
Research evidence suggests that the continuous process of ovulation and the resulting trauma to the ovary may play a role in the development of ovarian cancer.
Each cycle of ovulation causes a minor injury to the ovary as an egg is released, which then needs to be repaired. It’s hypothesized that repeated cycles of injury and repair could lead to DNA errors and potentially cancer over time.
This theory is supported by the reduced risk of ovarian cancer observed in women who have taken oral contraceptives, which suppress ovulation.
Despite the potential for certain cysts to become cancerous, it’s important to note that the vast majority of ovarian cysts are benign and resolve on their own. Regular gynecological exams and monitoring of any changes or symptoms can help in the early detection of both cysts and cancer.
For cysts that do not resolve or appear suspicious on ultrasound, further evaluation and sometimes surgery may be recommended to determine their nature and prevent any potential complications.
In conclusion, while ovarian cysts and ovarian cancer can affect the same organs, the presence of cysts does not necessarily indicate cancer. Understanding the differences between these conditions and their potential relationship is crucial for women’s health awareness.
Regular medical check-ups, awareness of the symptoms, and understanding personal risk factors are key strategies for the early detection and management of both ovarian cysts and cancer.
Armed with knowledge, women can navigate the complexities of ovarian health with confidence and advocate for their well-being.
If you care about cancer, please read studies about a new method to treat cancer effectively, and this low-dose, four-drug combo may block cancer spread.
For more information about cancer prevention, please see recent studies about nutrient in fish that can be a poison for cancer, and results showing this daily vitamin is critical to cancer prevention.
Copyright © 2024 Knowridge Science Report. All rights reserved.



