In a groundbreaking study published in Nature Genetics, researchers led by the Mead Group at the Radcliffe Department of Medicine have unveiled a new layer of complexity in how mutations in the TP53 gene interact with inflammation to give rise to an aggressive form of leukemia.
The TP53 gene, commonly known as the “guardian of the genome,” is the most frequently mutated gene in human cancers.
Hematopoietic Stem Cells: The Starting Point of Blood Cells and Leukemia
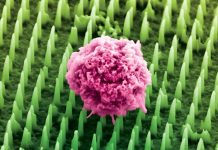
Hematopoietic stem cells (HSCs) are responsible for producing all blood cell types, serving as a cornerstone for a healthy blood system.
When the body faces inflammation, these stem cells usually differentiate into white blood cells to help combat infection.
However, mutations in the TP53 gene cause these stem cells to behave unpredictably, leading to a greater likelihood of cancer progression, specifically acute myeloid leukemia.
The Destructive Synergy of TP53 Mutations and Inflammation
Until now, the process by which TP53-mutated HSCs contribute to the development of leukemia was not fully understood.
This new study reveals that inflammation causes the selective expansion of TP53-mutant cells, disrupting their normal differentiation process.
In individuals with a healthy TP53 gene, inflammation usually triggers programmed cell death to prevent the spread of damaged cells.
In the case of TP53 mutations, this failsafe is bypassed, and instead, the stem cells proliferate uncontrollably, further advancing cancer progression.
A Novel Methodology: TARGET-seq
The research team utilized a state-of-the-art method known as TARGET-seq to analyze single cells, enabling them to distinguish which HSCs carried a TP53 mutation and how these cells behaved during disease progression.
The researchers found that the TP53-mutant cells showed activation of genes related to inflammatory processes.
Experiments on mice confirmed that inflammation boosted the number of TP53-mutant cells, which further resisted cell death induced by inflammation.
Genetic Integrity at Risk
The study also revealed that TP53 mutations change how cells repair genetic errors, making them more prone to mutations that accelerate cancer development.
In essence, TP53 mutations and inflammation create a vicious cycle that speeds up the onset of aggressive leukemia.
Implications for Cancer Treatment and Future Research
Dr. Alba Rodriguez-Meira, one of the paper’s co-authors, emphasized that these findings offer crucial insights into the intertwined roles of genetic mutations and inflammation in blood cancer.
“This could pave the way for better methods of early detection and new treatments for TP53-mutant leukemia and many other cancer types,” she said.
Professor Adam Mead echoed the significance of the study: “The connection between inflammation and genetic evolution in cancer has broad implications, and the challenge now is to intervene in this process to treat or even prevent the progression of cancer.”
Conclusion
This revolutionary study highlights the intricate relationship between chronic inflammation and genetic mutations in the development of aggressive leukemia.
Its findings may lead to improved early detection methods and new treatments, offering a ray of hope for countless patients grappling with TP53-mutant cancers.
If you care about health please read studies that vitamin D can help reduce inflammation, and vitamin K could lower your heart disease risk by a third.
For more information about health, please see recent studies about new way to halt excessive inflammation, and results showing foods that could cause inflammation.
The research findings can be found in Nature Genetics.
Follow us on Twitter for more articles about this topic.
Copyright © 2023 Knowridge Science Report. All rights reserved.