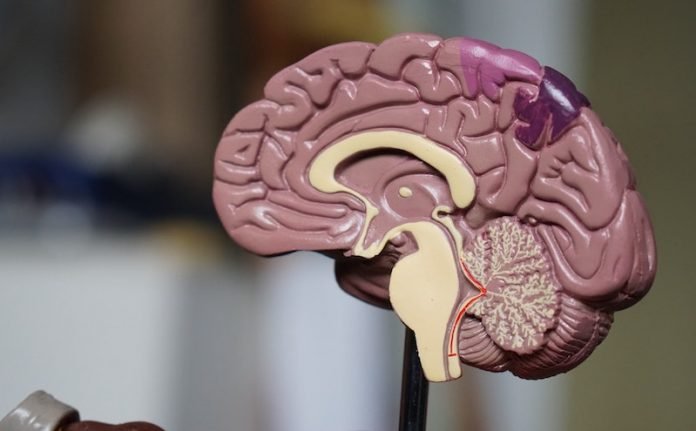
Frontotemporal disorders (FTD), sometimes called frontotemporal dementia, are the result of damage to neurons in the frontal and temporal lobes of the brain.
Many possible symptoms can result, including unusual behaviors, emotional problems, trouble communicating, difficulty with work, or difficulty with walking.
FTD is rare and tends to occur at a younger age than other forms of dementia. Roughly 60% of people with FTD are 45 to 64 years old.
FTD is progressive, meaning symptoms get worse over time. In the early stages, people may have just one symptom.
As the disease progresses, other symptoms appear as more parts of the brain are affected. It is difficult to predict how long someone with FTD will live.
Some people live more than 10 years after diagnosis, while others live less than two years after they are diagnosed.
There is currently no cure for FTD, and no treatments slow or stop the progression of the disease, but there are ways to help manage the symptoms.
In the early stages, it can be hard to know which type of FTD a person has because symptoms and the order in which they appear can vary from one person to another. Also, the same symptoms can appear across different disorders and vary from one stage of the disease to the next as different parts of the brain are affected.
Symptoms of FTD are often misunderstood. Family members and friends may think that a person is misbehaving, leading to anger and conflict.
It is important to understand that people with these disorders cannot control their behaviors and other symptoms and lack any awareness of their illness.
There are three types of frontotemporal disorders (FTD): behavioral variant frontotemporal dementia (bvFTD), primary progressive aphasia (PPA), and movement disorders.
FTD can be hard to diagnose because the symptoms are similar to those of other conditions. For example, bvFTD is sometimes misdiagnosed as a mood disorder, such as depression.
To make matters more confusing, a person can have both FTD and another type of dementia, such as Alzheimer’s disease.
Also, because these disorders are rare, physicians may be unfamiliar with the signs and symptoms.
To help diagnose frontotemporal dementia, a doctor may:
- Perform an exam and ask about symptoms
- Look at personal and family medical history
- Use laboratory tests to help rule out other conditions
- Order genetic testing
- Conduct tests to assess memory, thinking, language skills, and physical functioning
- Order imaging of the brain
A psychiatric evaluation can help determine if depression or another mental health condition is causing or contributing to the condition.
Only genetic tests in familial cases or a brain autopsy after a person dies can confirm a diagnosis of FTD.
Researchers are studying ways to diagnose FTD earlier and more accurately and to distinguish them from other types of dementia.
One area of research involves biomarkers, such as proteins or other substances in the blood or cerebrospinal fluid which can be used to measure disease progression or the effects of treatment.
Researchers are also exploring ways to improve brain imaging and neuropsychological testing.
If you care about dementia, please read studies about your walking speed may tell your risk of dementia, depression, and more, and findings of high blood pressure drugs that could prevent dementia.
For more information about brain health, please see recent studies about this common nutrient may protect your brain, preventing dementia, and results showing this supplement could keep dementia at bay.



