What is it? Molnupiravir, also known by the brand name Lagevrio, was developed by Merck and Ridgeback Biotherapeutics.
It was heralded as a potential game-changer when the companies announced their initial clinical trial results in 2021.
But when the data was finalized, it showed the drug to have lower efficacy than originally reported.
Its FDA authorization came after a close vote that took into account the lowered efficacy and safety profile.
The Centers for Disease Control & Prevention (CDC) now recommends that this drug should be used when the above-mentioned treatments aren’t available.
When it was authorized: December 2021.
Who can get it: People ages 18 and up who are at high risk for hospitalization and death from COVID-19.
How you take it: Four capsules every 12 hours (for example, at 8 a.m. and 8 p.m.) for five days. It must be taken as soon as possible, within five days of symptom onset.
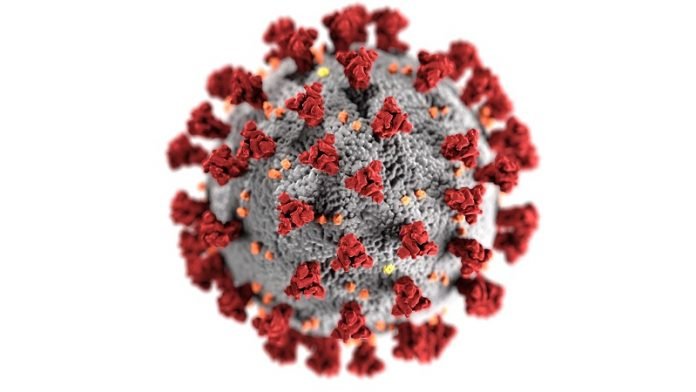
How it works: When the drug enters the bloodstream, it blocks the ability of the SARS-CoV-2 virus to replicate.
How well it works: 30% efficacy against hospitalization and death. Merck initially reported the efficacy as 50%, but later adjusted that figure.
Some laboratory studies from Merck have shown that molnupiravir is effective against the Omicron variant.
Side effects: Diarrhea, nausea, and dizziness are the most common side effects. You should stop taking the pills right away if you have an allergic reaction.
Because molnupiravir is still being studied, it’s possible that all of the risks aren’t yet known.
What else you should know: Molnupiravir is not recommended during pregnancy, since it has not been studied in pregnant women and has shown potential harm in in vitro studies—therefore, the true risk for harm to an unborn baby is unknown.
Individuals who are able to become pregnant should use reliable birth control during treatment and for four days after their last dose.
It is also not known if molnupiravir could affect sperm, so individuals who are taking molnupiravir and who are sexually active with partners who are able to become pregnant should use reliable birth control during treatment and for three months after the last dose.
(Studies to understand the risk to sperm beyond three months are ongoing.)
The NIH considers this to be an alternative treatment, which should be used only when neither of the NIH-preferred therapies (Paxlovid and remdesivir) are available, feasible to use, or clinically appropriate.
If you care about COVID, please read studies about why people with blood Type O less likely to get COVID-19, and this low-cost drug can treat COVID-19.
For more information about COVID, please see recent studies about new drug that could prevent COVID-19, and results showing current COVID-19 vaccines cannot effectively prevent omicron infection.



