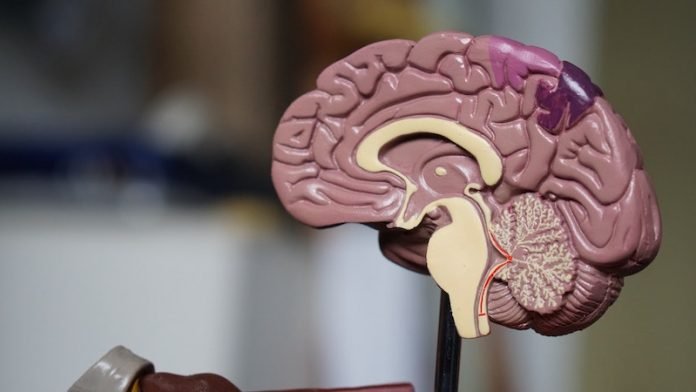
researchers did a comprehensive review of the COVID-19’s effect on the nervous system which classifies brain damage caused by COVID-19 into three stages.
They encourage the adoption of this three-stage classification, call for more research on COVID’s long-term effects on the brain, and stress the need for patients to receive a brain MRI before leaving the hospital.
The research was conducted by a team at Johns Hopkins Medicine and elsewhere.
Scientists are learning that a large number of hospitalized COVID-19 patients have various degrees of brain impairment.
The team says as a medical community, researchers need to monitor these patients over time as some of them may develop cognitive decline, attention deficit, brain fog, or Alzheimer’s disease in the future.
There is a lot we can do to promote brain healing in COVID-19 patients, but first, they must understand the nature and severity of their neurological deficits.
At the patient level, getting a baseline MRI before leaving the hospital is imperative so that we have a starting point to evaluate and treat them.
In the paper, the team warns about neurological issues in patients who suffer from COVID-19, including stroke, seizures, confusion, dizziness, paralysis, and/or coma.
Already, two dozen case reports are revealing the impact of COVID-19 on the brains of patients. In fact, one study from Wuhan, China, showed that 45% of patients with severe COVID-19 illness experience marked neurological deficits.
Another study from France showed 84% of ICU patients with COVID-19 have positive abnormalities on their neurological examination, and that 15% of patients who leave the ICU have residual “dysexecutive function,” which involves poor attention and difficulty with decision-making and controlling behavior.
The paper proposes the adoption of a three-stage “NeuroCovid” classification scheme to provide a basis from which to build on future hypotheses and investigations regarding SARS-Cov2 and the nervous system.
These stages include:
NeuroCovid Stage I: The virus damage is limited to epithelial cells of nose and mouth and the main symptoms include transient loss of smell and taste.
NeuroCovid Stage II: The virus triggers a flood of inflammation, called a cytokine storm, which begins in the lungs and travels in the blood vessels throughout all body organs.
This cytokine storm leads to the formation of blood clots which cause small or large strokes in the brain.
NeuroCovid Stage III: An explosive level of cytokine storm damages the blood-brain barrier, the protective insulation layer in blood vessels of the brain.
As a result, blood content, inflammatory markers, and virus particles invade the brain and patients develop seizures, confusion, coma, or encephalopathy.
The team points out that many patients with COVID-19 may have no noticeable neurological symptoms at first; but in some cases, patients may present with neurological symptoms even before they have fever, cough, or shortness of breath.
In addition to having an MRI while at the hospital, the team stresses that patients will need to be monitored in a few months after their hospitalization.
Findings from studies about previous forms of coronaviruses suggest that in the long-term patients may develop depression, insomnia, Parkinson’s disease, memory loss, or accelerated aging in the brain
For those recovering from COVID-19, the team recommends regular exercise, eating a heart-healthy diet, reducing stress, and improving sleep; these are critical ways patients can rejuvenate their brain and minimize having poor outcomes in the future.
One author of the study is nationally-recognized neurologist Dr. Majid Fotuhi, MD, Ph.D.
The study is published in the Journal of Alzheimer’s Disease.
Copyright © 2020 Knowridge Science Report. All rights reserved.



