In a new study, researchers reported that using brain circuits made in silicon, they have reduced symptoms of heart failure by reinstating the body’s natural heart rhythm.
This finding holds great potential for designing more effective pacemakers in the future.
The research was conducted by a team at the Universities of Bath and Bristol.
In the UK alone, around 900,000 people are living with heart failure and almost 1.4 million have survived a heart attack.
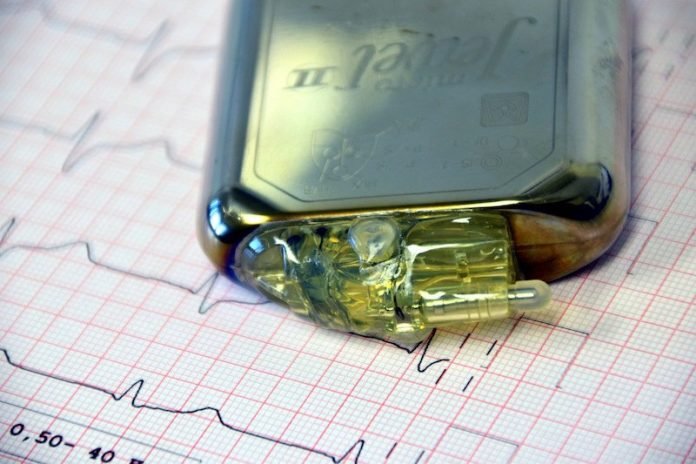
After such an event, pacemakers are often fitted to either speed up the heart or to overcome electrical conduction problems between different chambers of the heart.
There is no cure for heart failure; its progression is only slowed by current medication.
The heartbeat is never constant; it varies with every breath. It speeds up when you inhale and slows down when you exhale. This difference in heart rate is known as respiratory sinus arrhythmia.
In the study, the researchers have adopted this arrhythmia in a novel bionic pacemaker and applied it to a heart in heart failure.
They found that this new form of heart pacing dramatically increases the efficiency of the heart.
Normally, pacemakers don’t listen to signals from our bodies; they simply pace the heart at a monotonous, regular rate.
These researchers, however, built a pacemaker that read the body’s own breathing signals to speed up and slow down the heart every breath.
They used state-of-the-art high-resolution echocardiography to monitor the heart’s performance during respiratory sinus arrhythmia pacing in rats with heart failure.
Within two weeks there was a 20% increase in blood pumped by the heart which was not the case when we used conventional pacemakers.
This approach may represent a novel therapy in addition to those already available for the treatment of heart failure.
The team says the findings give hope for heart failure patients and may revolutionize the future design of cardiac pacemakers.
The next step in the research is to find out if respiratory sinus arrhythmia can reverse heart failure in human patients, as it has done in rats.
The lead author of the study is Dr. Erin O’Callaghan.
The study is published in The Journal of Physiology.
Copyright © 2019 Knowridge Science Report. All rights reserved.



