Women with urological problems might not know how common — and treatable — they are, which keeps them from seeking proper care.
But help is available.
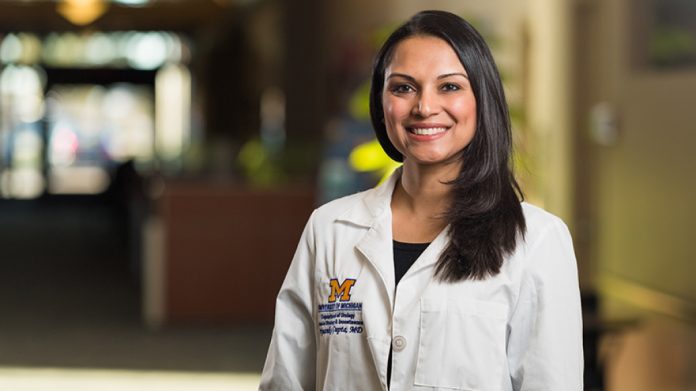
“I think there are a lot of women who live with these issues and don’t realize there are resources or things they can do to improve their quality of life,” said Priyanka Gupta, M.D., a Michigan Medicine urologist and an assistant professor of urology.
Another potential deterrent: About 89% of urologists are men.
A urologist’s gender shouldn’t prevent a woman from making an appointment, Gupta says. She knows, however, that some patients might prefer to see a female practitioner who understands their issues firsthand.
“There’s a level of comfort,” she said.
That thinking guides her role at the Women’s Urology Clinic at Michigan Medicine. The practice, based in Chelsea and at the Livonia Center for Specialty Care in suburban Detroit, treats women of all ages.
Gupta explains the concerns she hears from patients and how she helps address them:
Incontinence after pregnancy
The scenario: This unintentional leakage after laughing, coughing, sneezing or jumping most often occurs in women in their late 30s and older, typically after having children, Gupta says.
Excess bodyweight can also contribute to developing leakage.
The solution: Gupta begins with a physical exam and evaluation.
Opting for the “least invasive thing first,” she’ll discuss physical and behavioral therapies, including reducing water and caffeine intake as well as trying exercises for the pelvic floor muscles to build strength.
Surgical options are available if the problem persists or worsens.
Overactive bladder
The scenario: Having to pee at all hours and with little warning can be a nuisance.
The cause, Gupta says, typically is simply a side effect of growing older — and it affects men and women alike.
Although doctors still aren’t sure what causes it, lifestyle factors such as caffeine intake, drinking habits and diuretic medications that rid the body of water can play a role.
The solution: Behavioral modifications come first: cutting caffeine and alcohol and, if possible, altering the time of taking a diuretic.
Physical therapy and medications also are considered.
Gupta may suggest nerve therapy, which involves a needle placed in the ankle (“kind of like acupuncture”) to transmit electric stimulation targeting the nerves that control bladder function.
More invasive options include Botox injections and an implantable bladder pacemaker.
Urinary tract infection
The scenario: It’s the most common condition Gupta sees: painful, sometimes cloudy or foul-smelling urine, often accompanied by urgency, frequency, burning and pain with urination — and often occurring several times a year.
But Gupta says women too frequently receive antibiotics for this issue without confirming a UTI (a practitioner might also miss an overlapping issue, such as overactive bladder).
Worse, antibiotic resistance can develop if overprescribed.
The solution: Gupta helps women determine what might be causing a relapse. “Fluid intake is important, as is managing your bowels,” Gupta said. “Constipation can be a big contributor.”
She also rules out anatomic problems that may be a factor.
Research, Gupta adds, has shown the benefit of vaginal estrogen cream for postmenopausal women to alter their pH levels and promote healthy bacterial growth.
Gupta consults with a patient at the Michigan Medicine Women’s urology clinic.
Pelvic floor dysfunction
The scenario: The pelvic floor is a “bowl” of muscles supporting the bladder, vagina and rectum.
Noted Gupta: “Those muscles, particularly after childbirth, get disrupted and can become irritated and inflamed.”
The muscles need to relax to urinate well and pass a bowel movement.
Tension also can cause pain during intercourse, painful or frequent urination and lower back pain.
The solution: Because most women aren’t taught how to relax those muscles, some proactive effort is required.
Gupta typically directs a patient toward pelvic floor therapy — weekly sessions that help a woman identify and unclench the affected area (“Some people hold stress in their pelvis and don’t even realize it,” she said.)
Vaginal medications or muscle injections may help, too.
Pelvic organ prolapse
The scenario: Weak spots in the walls and muscles of the vagina can cause adjacent organs to fall out of their normal positions — “essentially a hernia of the vagina,” Gupta said.
Our best understanding is that injury to the pelvic floor muscles during childbirth causes the loss of support and prolapse.
Signs of trouble: a sensation of a bulge in the vagina or discomfort when sitting.
The solution: If the patient is bothered or in pain, surgery can follow.
Still, said Gupta, “it’s not a condition that has to be surgically corrected; it all depends on the patient’s symptoms.”
A silicone or rubber diaphragm (known as a pessary) inserted into the vagina to support the pelvic floor is an option as well.
Written by Kevin Joy.
If you care about health, please read studies about how Mediterranean diet could protect your brain health, and the best time to take vitamins to prevent heart disease.
For more health information, please see recent studies that olive oil may help you live longer, and vitamin D could help lower the risk of autoimmune diseases.



