Researchers from Weill Cornell Medicine have discovered how COVID-19 can cause new cases of diabetes or worsen existing diabetes in infected individuals.
Using a cutting-edge model, the team found that the virus responsible for COVID-19, SARS-CoV-2, triggers an immune response that damages the pancreas, specifically the cells responsible for producing insulin.
The study was published in the journal Cell Stem Cell.
Dr. Shuibing Chen, one of the lead authors and director of the Center for Genomic Health at Weill Cornell Medicine, explained that some viral infections, including COVID-19, have long been suspected of triggering type 1 diabetes.
This study provides evidence of how this process occurs.
The pancreas contains specialized cells called beta cells that produce insulin, a hormone necessary to regulate blood sugar levels.
When COVID-19 patients were examined, doctors noticed damage to the pancreas, alongside effects on other organs like the lungs, heart, and liver.
To explore this further, researchers studied pancreatic tissue samples from people who had died from COVID-19.
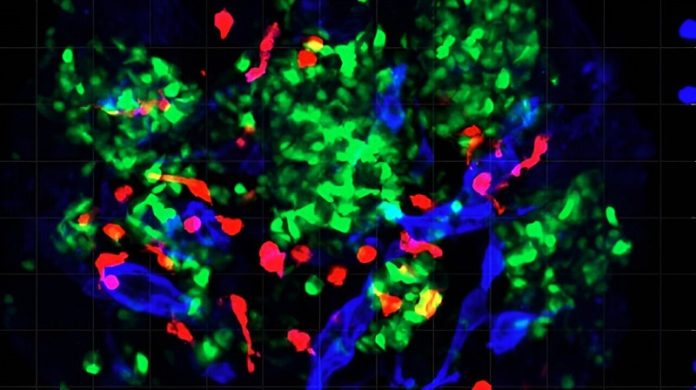
The team used a high-tech analysis technique, GeoMx, to examine the pancreas in detail. They found that immune cells known as proinflammatory macrophages were present in the damaged tissue.
These cells typically fight infections by killing pathogens, but they can also cause harm to healthy tissue when activated incorrectly.
To better understand this, the researchers used a new model developed in the Chen Lab called pancreatic islet organoids.
These are tiny, lab-grown versions of the pancreas that contain both blood vessels and immune cells. The team infected the organoids with SARS-CoV-2 and observed that the macrophages were killing off the beta cells using a process known as pyroptosis, a form of cell death.
In addition to studying COVID-19, the team also looked at how another virus, coxsackievirus B4—known to play a role in type 1 diabetes—affected the pancreatic islets.
They found a similar macrophage-driven response, further supporting the idea that viral infections can trigger diabetes by damaging insulin-producing cells.
This discovery could help in the development of new treatments to protect the pancreas from viral damage. Although it is too early to test any therapies, the study provides a foundation for future research.
The findings may also offer insights into long COVID, a condition affecting millions of people who continue to experience symptoms long after recovering from the initial infection.
Dr. Robert Schwartz, a co-author of the study, emphasized the importance of these findings, noting that while the immediate priority for COVID-19 patients is to address life-threatening symptoms, understanding how the virus affects organs like the pancreas is key for long-term health strategies.
If you care about diabetes, please read studies about 5 vitamins that may prevent complication in diabetes, and how to manage high blood pressure and diabetes with healthy foods.
For more health information, please see recent studies about vitamin D and type2 diabetes, and to people with type 2 diabetes, some fruits are better than others.



