Thousands of Americans experience blood clots every year.
Knowing if you’re at risk and what symptoms to look out for are important to ensure you get prompt treatment.
As a nurse practitioner at the Michigan Medicine Frankel Cardiovascular Center, my heart patients often come to me with questions about blood clots, also known as deep vein thrombosis.
Here are answers to some of the most common questions I’m asked.
- What is a blood clot?
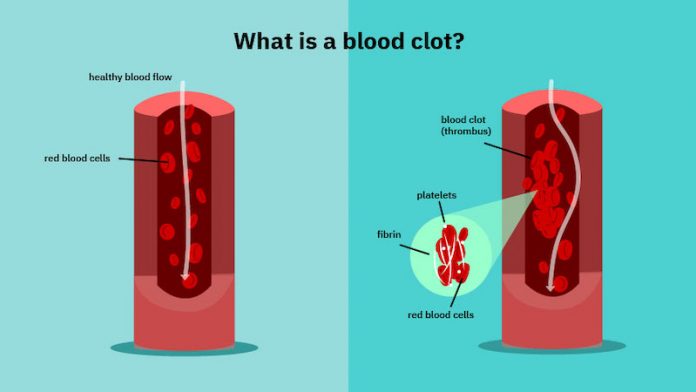
A blood clot is a collection of blood in the body that has changed from liquid to a semi-solid mass.
The body does this to stop bleeding when injured, but sometimes a clot forms inside a blood vessel and does not dissolve on its own.
Platelets — cells that float in the blood — become sticky in response to injury and begin to attach to one another as well as to a blood vessel wall.
Next, web-like strands in the blood, called fibrin, attach to the platelets and form a net that traps red blood cells.
This reaction usually stops when the injury is repaired, and the body breaks down the clot. Sometimes, the action continues and becomes a blood clot that prevents blood from flowing through that vessel.
The most common type of blood clot is called deep vein thrombosis or DVT. This is a clot in one of the deep veins of the body, usually in the leg.
When the clot is new, a piece of it can break off and travel to the lungs. This is known as a pulmonary embolism.
- What are the symptoms of a blood clot?
Symptoms of a DVT include swelling of the affected leg, pain, redness, warmth and new visible veins in the area.
Symptoms of a pulmonary embolism include shortness of breath, chest pain, cough or coughing up blood and fast breathing.
Although these symptoms can be associated with many different health problems, if you suspect you have a clot, call your health care provider right away or go to the nearest emergency room.
- How is a blood clot diagnosed?
Your provider will ask you a series of questions. If a blood clot is suspected, you will likely undergo one of these tests:
A blood test called a d-dimer. This is a compound released from blood clots. It is high when you have a new clot.
An ultrasound of the leg. This uses sound waves to watch blood flow in the veins.
A CT scan of the chest if a pulmonary embolism is suspected.
- What causes a blood clot?
Many risk factors and illnesses increase your risk of getting a blood clot. Risk factors include:
Inactivity related to an injury or a long car or plane trip
Having surgery or being in the hospital for an extended period
Damage to your blood vessel from an injury
Taking some medications such as birth control pills
Inherited blood clotting tendencies
Cancer
Pregnancy
Being over 60 years’ old
Obesity
- Why do those factors increase the risk of a blood clot?
Much of the risk is due to blood flow slowing down when you’re not able to move around. Blood that is stagnant or still tends to clot.
Injury also causes a reaction in your blood that increases the risk of clotting. The genetic makeup of your blood, as well as illness, can also make clotting more likely.
- How can I prevent blood clots?
The best way to prevent blood clots is to stay active and avoid sitting for long periods of time. Other things to keep in mind:
When traveling by car or plane, take frequent breaks and move around.
Maintain a good body weight and stay hydrated.
Don’t smoke.
Talk to your doctor about preventing clots after surgery.
Know your family history of blood clotting.
- How is a blood clot treated?
If you’re diagnosed with a blood clot, you may have to take a blood thinning medication, also called an anticoagulant.
This type of medication stops the clot from growing and allows your body to break it down naturally, before it can travel to other areas of your body.
If the clot is very large or life threatening, you may need to be hospitalized to receive clot-dissolving medication or to get a clot removal.
Blood thinners are usually prescribed for three months, or until the health issue that caused the clot is gone.
The decision of when to stop taking your blood thinning medication should be made with your doctor.
- Once I have a blood clot, am I more likely to have another one?
A blood clot sometimes leaves a scar in the vein where it occurred. This makes the vein “abnormal” or different and more likely to clot again.
Being aware of this risk and taking the necessary precautions helps to prevent another clot.
- How are COVID-19 patients treated to prevent blood clots?
Patients who are hospitalized with COVID infection are at high risk for blood clots. They may be treated with blood thinners while they are in the hospital, and some for a short time after.
The risk of blood clots is assessed in everyone who is admitted to the hospital. If your risk is high, you will receive low doses of blood thinners while in the hospital.
- I have COVID-19 – am I at risk for blood clots?
Patients with COVID infection who are not hospitalized do not seem to have a high risk of blood clots.
Talk to your doctor about your concerns and keep an eye on the symptoms listed above, getting care immediately if you’re concerned.
Written by Clare Harris, NP.



