One of the hardest challenges for people recovering from addiction is avoiding relapse.
Even after long periods of abstinence, the brain’s wiring often pulls people back toward drug use.
A new study from the University of North Carolina at Chapel Hill has uncovered a surprising reason why this happens—and a potential new way to prevent it.
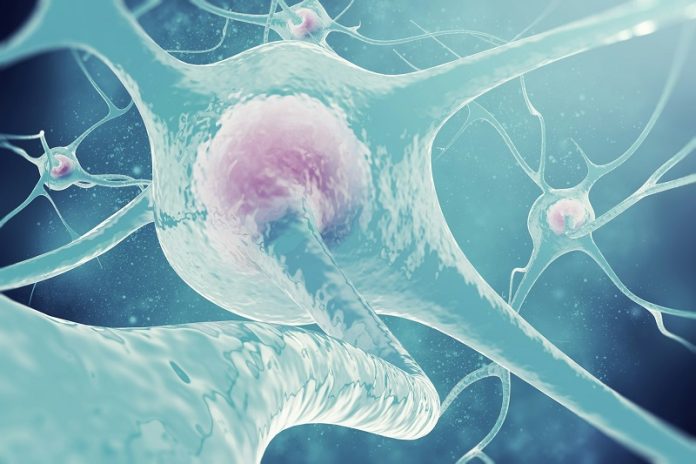
Researchers found that the brain’s immune cells, called microglia, play an unexpected role in relapse. Using a rodent model of cocaine use, they discovered that during abstinence, microglia begin attacking and pruning parts of nearby support cells called astrocytes.
These star-shaped cells help regulate the brain’s reward circuits, which are deeply involved in craving and drug-seeking behaviors.
When astrocytes were damaged, drug-seeking behaviors became stronger. But when scientists blocked the microglia from stripping away astrocyte connections, relapse behaviors were reduced.
“Our findings reveal that brain immune cells can drive drug craving by stripping away support structures that keep neural circuits balanced,” said Kathryn Reissner, lead investigator and professor of psychology and neuroscience at UNC.
“By protecting these connections, we may be able to reduce relapse risk in people recovering from addiction.”
Astrocytes had long been known to shrink after repeated cocaine use, but the cause of that damage wasn’t understood until now.
This is the first study to show that the brain’s own immune system is responsible—and that this immune response directly contributes to relapse risk.
Traditionally, addiction research has focused on neurons, the brain’s main signaling cells. But this study highlights the importance of other cell types.
“Addiction treatments have long focused on neurons, but this work shows that targeting the brain’s immune system could open an entirely new front in the fight against addiction and relapse,” said co-lead researcher Anze Testen.
The findings suggest that future therapies could focus not only on supporting neurons but also on protecting astrocytes and regulating immune activity in the brain.
“By understanding how microglia and astrocytes interact after drug use, we’re closer to designing targeted strategies to help people stay drug-free,” said Jonathan VanRyzin, a co-lead author of the study.
Although this research was conducted in animals, it points to a broader principle: the brain’s immune system may be deeply involved in how the brain adapts after substance use.
Researchers hope to explore whether the same process occurs in people with substance-use disorders.
If so, treatments could one day block harmful immune activity in the brain, helping people maintain recovery and break the cycle of relapse.
If you care about brain health, please read studies about a simple solution to fight dementia and big causes of memory loss, dementia you need to know.
For more health information, please read studies that people who take high blood pressure medications have lower dementia risk and early indicators of dementia: 5 behaviour changes to look for after age 50.



