For over 100 years, doctors and health experts have used the International Classification of Diseases (ICD) to name and organize different illnesses and causes of death.
This system helps collect health data, track disease patterns, and improve medical care. The ICD assumes each disease is separate, but scientists are now realizing that some health problems may be connected.
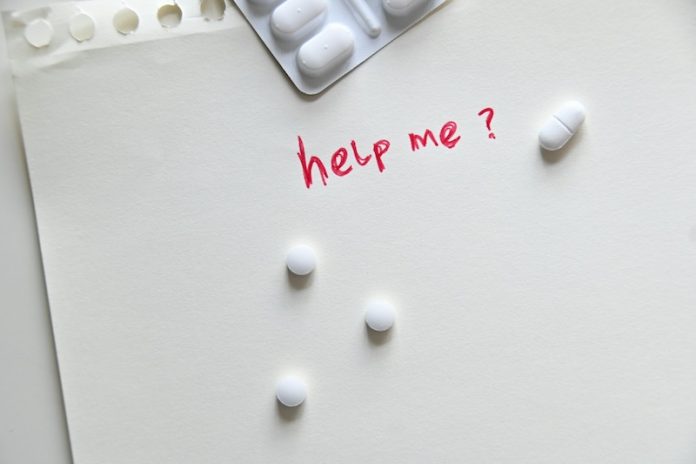
One example is “deaths of despair,” a term that describes deaths caused by suicide, drug overdoses, and alcohol-related diseases. These deaths often happen when people struggle with serious problems like financial difficulties, social isolation, or mental health issues.
A team of researchers from Florida Atlantic University studied trends in deaths of despair in the U.S. between 1999 and 2021. They focused on people aged 25 to 74 and looked at how these deaths changed over time. The study used 19 different causes of death related to substance use, mental health, and liver disease.
Their findings paint a troubling picture: deaths of despair have sharply increased in the last two decades. By 2021, they had risen 2.5 times compared to 1999.
If counted as a single category, deaths of despair would be the fifth leading cause of death in the U.S., behind heart disease, cancer, COVID-19, and accidents. That year, 176,386 people died from suicide, drug overdoses, or alcohol-related conditions.
The researchers used official death records from the Centers for Disease Control and Prevention (CDC) to track these numbers. They noted that these deaths do not affect all groups equally. By 2022, the rate of deaths of despair among Black Americans had become higher than among white Americans.
The highest rates were found among American Indian and Alaska Native populations, who often face significant economic and social challenges.
Experts believe that stopping this crisis will require more than just medical care. A combination of mental health support, substance abuse treatment, and social changes is needed.
Maria Carmenza Mejia, one of the study’s authors, explained that research must continue to find out why these deaths are rising and how to prevent them. She also suggested that doctors and policymakers should consider factors like poverty, education, and social support when treating and preventing these conditions.
Another researcher, Panagiota Kitsantas, emphasized the importance of making mental health and addiction treatment part of regular healthcare. She suggested that if people could get help from their primary doctors instead of seeking separate treatment, it could reduce stigma and make care more accessible.
Analysis of the Findings
This study highlights a serious and growing problem. The number of deaths caused by despair has increased dramatically, showing that many people in the U.S. are struggling with deep personal and social challenges.
While medical conditions like heart disease and cancer remain the leading causes of death, deaths related to mental health and substance abuse are rising fast and affecting more people.
A key takeaway is that economic and social factors play a big role in these deaths. People in communities facing poverty, discrimination, or lack of healthcare are more at risk. The fact that death rates are highest among Native American populations shows the impact of long-standing social inequalities.
The study also suggests that changing the way we classify diseases could help. Right now, the ICD treats conditions like liver disease, drug addiction, and suicide separately. But if they were seen as related, doctors and health officials could take a more comprehensive approach to preventing them.
In the end, the findings make it clear that deaths of despair are not just a medical issue—they are a social crisis. Tackling this problem will require action at all levels, from individual support and medical care to broader economic and policy changes.
The research findings can be found in Advances in Preventive Medicine and Health Care.
Copyright © 2025 Knowridge Science Report. All rights reserved.



