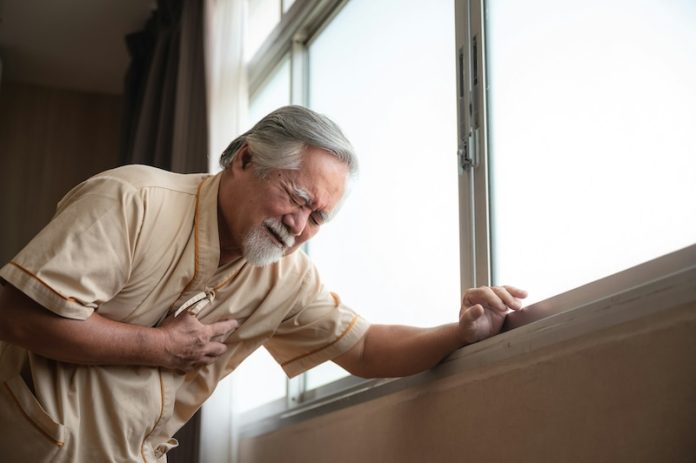
Sudden cardiac arrest (SCA) is a life-threatening condition where the heart abruptly stops pumping blood, leading to collapse and often death if immediate action isn’t taken.
It’s one of the leading causes of death, responsible for 50% of cardiac-related deaths and 20% of all fatalities in high-income countries. For individuals with type 2 diabetes (T2D), the risk of SCA is even higher—about twice that of the general population.
A recent study presented at the European Association for the Study of Diabetes (EASD) meeting in Hamburg has shed light on factors that might elevate the risk of SCA in people with T2D.
These include certain medications, low blood sugar, and other health conditions, many of which might not be well-known among healthcare providers.
Researchers, led by Peter Harms from Amsterdam UMC, conducted a case-control study to identify characteristics associated with SCA in people with T2D.
The study involved 3,919 individuals, including 689 who had experienced SCA and 3,230 who had not.
Each case was matched with up to five controls based on age, sex, and general practitioner (GP) practice. Researchers reviewed medical records spanning five years before the SCA events to identify potential risk factors.
The study highlighted several factors linked to an increased risk of SCA in T2D patients. These include:
- History of arrhythmias: Individuals with a history of irregular heartbeats had a 68% higher risk of SCA.
- Unknown smoking status: Not knowing whether a patient smoked was linked to a 40% higher risk.
- Insulin use: People on insulin therapy faced a 138% higher risk of SCA.
- Medications that prolong the QT interval: Certain drugs, like prokinetics and antipsychotics, that affect heart rhythm increased the risk by 66%.
For patients with a history of cardiovascular disease (CVD), additional factors like moderate or severe kidney damage (albuminuria) and heart failure were linked to higher SCA risk. In contrast, for those without CVD, risks included:
- Low fasting glucose levels (indicating overly strict blood sugar control)
- Severely high systolic blood pressure
- Low HDL (“good”) cholesterol and high LDL (“bad”) cholesterol
- Use of antibiotics and antipsychotic medications that affect heart rhythm
Many GPs are already aware that traditional cardiovascular risk factors, such as high blood pressure, contribute to SCA risk in T2D patients. However, this study brings attention to less obvious risks, like low fasting glucose levels and the use of certain medications.
Peter Harms emphasized the importance of recognizing these risks, particularly the dangers of overly strict blood sugar control and the impact of commonly prescribed antibiotics, antipsychotics, and prokinetics.
Striking the right balance in managing blood sugar and medications is essential to reduce the likelihood of SCA in T2D patients.
This study highlights the need for a more tailored approach to treating T2D patients. By understanding the nuanced risks that certain treatments and conditions pose, healthcare providers can make more informed decisions about medication and glycemic control strategies.
Simple adjustments—like avoiding excessively low blood sugar levels, carefully choosing medications, and monitoring cardiovascular health—could make a significant difference in preventing SCA.
Enhanced awareness among GPs and other healthcare professionals could pave the way for better prevention and management of this potentially deadly condition.
For patients, this research underscores the importance of regular check-ups and open communication with healthcare providers about medications, blood sugar targets, and overall health.
With the right approach, the risk of SCA can be minimized, offering a safer and healthier future for those living with T2D.
If you care about diabetes, please read studies about bananas and diabetes, and honey could help control blood sugar.
For more health information, please see recent studies about Vitamin D that may reduce dangerous complications in diabetes and results showing plant-based protein foods may help reverse type 2 diabetes.
Copyright © 2024 Knowridge Science Report. All rights reserved.



