A new study from the University of Pittsburgh has revealed a promising approach to treating periodontal disease (PD) by targeting the immune system.
The research, published in Proceedings of the National Academy of Sciences, suggests that modulating the immune response could help prevent or treat PD, a serious gum disease that can lead to tooth loss.
Traditionally, treatments for PD have focused on fighting bacteria.
However, senior author Dr. Charles Sfeir explains that bacteria alone do not cause the disease.
Instead, they trigger an immune response, leading to inflammation and bone loss around the teeth.
“If we can control the immune system, we can change the bacteria in the mouth and stop the disease from progressing,” said Dr. Sfeir, who is an associate professor at the Pitt School of Dental Medicine and a member of the McGowan Institute for Regenerative Medicine.
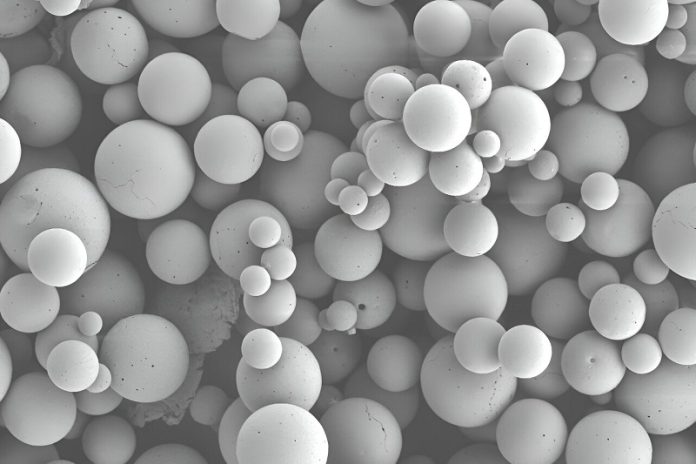
Dr. Sfeir collaborated with Dr. Steven Little, an expert in chemical engineering, to develop microparticles that release an immune-modulating compound called CCL2.
This compound helps shift the immune response away from inflammation, allowing the body to heal and protect against bone loss.
The study, led by Dr. Mostafa Shehabeldin, involved testing the therapy in mice with PD. To simulate the disease, the researchers tied a silk thread around the molars of the mice, which caused bacteria to build up and trigger inflammation that destroys bone around the teeth.
They then treated the mice with the CCL2 microparticles to see if it could prevent or reverse the damage.
The results were promising. Whether the CCL2 therapy was given at the same time as the disease was triggered, after the disease had started, or when the disease was already resolving, the treatment helped reduce bone loss and improved bone healing.
The key to this success was changing the behavior of immune cells called macrophages.
The treatment shifted the macrophages from an inflammatory state (M1 type) to a healing, anti-inflammatory state (M2 type), which helped reduce the damage caused by the disease.
In addition to influencing the immune system, the CCL2 therapy also changed the oral microbiome by reducing the overall bacterial load and limiting the growth of harmful bacteria linked to PD.
Dr. Sfeir is excited about the potential of this treatment for PD patients, especially those with aggressive forms of the disease that don’t respond to regular dental cleanings.
He hopes to begin clinical trials soon, using CCL2 as an additional treatment alongside traditional methods like antimicrobial therapies and dental cleanings.
“This research could impact many people who suffer from periodontal disease,” said Dr. Sfeir. “For those who still experience bone loss despite good oral hygiene, this new immune-modulating therapy could be a game-changer.”
The study also provides new insights into how the immune system and bacteria interact in the mouth, making it a valuable model for studying other immune-driven diseases.
If you care about gum health, please read studies about an important causes of tooth decay and gum disease, and common tooth disease that may increase risks of dementia.
For more information about gum health, please see recent studies about mouthwash that may increase your tooth damage, and results showing this diet could help treat gum disease.



