Researchers from the University of Massachusetts Amherst and UMass Chan Medical School have made a significant breakthrough in treating pancreatic cancer.
Their study, published in Science Translational Medicine, describes a new method that successfully shrinks and even clears tumors in mice.
This innovative approach combines a novel drug-delivery system with immune-boosting agents to target and attack pancreatic tumors.
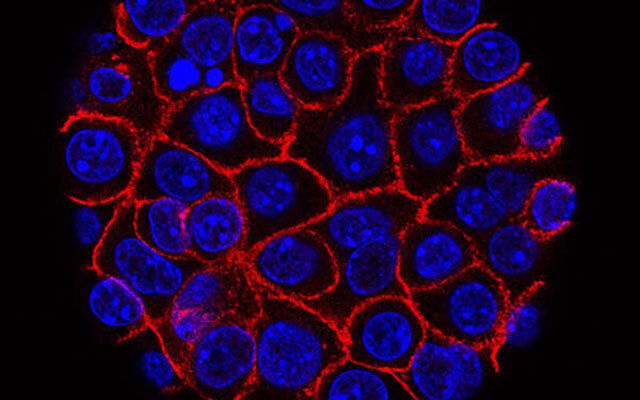
Pancreatic ductal adenocarcinoma (PDAC) is the most common type of pancreatic cancer and has a very low survival rate—only 13% of patients survive for five years after diagnosis. One of the main challenges in treating this cancer is its microenvironment, a dense tissue barrier that surrounds the tumor.
This barrier makes it difficult for drugs to reach the tumor and prevents the body’s immune cells from attacking it.
“Delivering drugs to these tumors is incredibly difficult because of the way the tissue around the tumor is structured,” explained Prabhani Atukorale, an assistant professor of biomedical engineering at UMass Amherst and co-lead author of the study.
This structure not only blocks drugs but also stops the immune system from recognizing and fighting the tumor.
Traditional treatments like chemotherapy and even newer immunotherapy approaches often fail against pancreatic cancer. But the researchers found a way to trick the immune system into attacking the tumor by targeting specific immune pathways. One of these pathways, called STING, usually responds to viral infections. By activating this pathway, the researchers were able to create a strong immune response against the tumor.
They also targeted another immune pathway, TRL4, which works together with STING to enhance the immune attack. However, getting these immune-activating agents through the tumor’s tough barrier was a challenge. To solve this, the researchers developed a new type of nanoparticle made from lipids (fat-based molecules) that can carry the immune agents directly to the tumor.
These nanoparticles are particularly effective because they can deliver both immune agents together, despite the fact that they normally don’t mix well. The nanoparticles ensure that the agents travel through the bloodstream together and are absorbed by the tumor cells at the same time.
When combined with a drug therapy known as T/P, this approach proved highly effective. In tests with mice, eight out of nine showed tumor shrinkage, and in two cases, the tumors disappeared completely. “This is remarkable,” said Marcus Ruscetti, co-lead author and assistant professor at UMass Chan Medical School. “We’ve never seen such results in this model before.”
Although the tumors returned after the mice were taken off the treatment, the study represents a promising step toward more effective therapies for pancreatic cancer. The researchers believe that this approach could also be applied to other types of cancer, such as colon, lung, and liver cancers.
This new treatment method is highly adaptable, meaning it can be customized for individual patients. “We can adjust the ratios of the immune agents and drugs to tailor the treatment to each patient,” said Atukorale.
The study also highlights the importance of collaboration between different scientific disciplines to develop innovative solutions for complex health problems.
If you care about cancer, please read studies about how to fight cancer with these anti-cancer superfoods, and a berry that can prevent cancer, diabetes and obesity.
For more health information, please see recent studies about how to harness the power of anti-cancer foods and supplements, and cancer-fighting foods and recipes.
Source: University of Massachusetts Amherst.



