A recent study in Europe has found a surprising link between a common drug for high blood pressure and an increased risk of sudden heart stoppage, also known as sudden cardiac arrest.
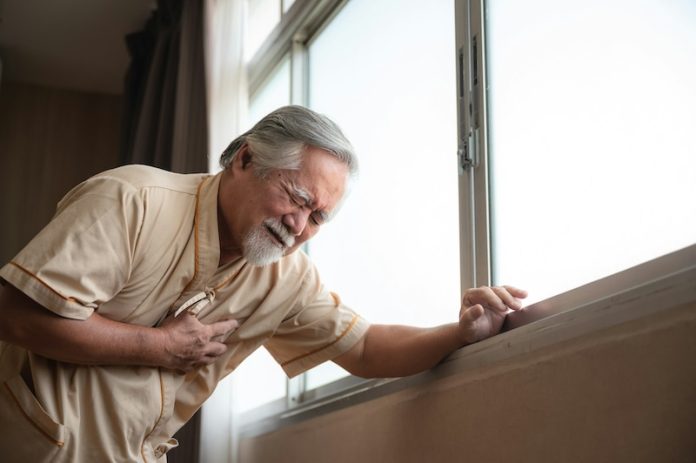
This condition happens when the heart suddenly stops pumping blood effectively, causing a loss of consciousness and, if not treated immediately, can lead to death. The drug in question is nifedipine, and researchers suggest that doctors and patients should use it with more caution.
Sudden cardiac arrest is a serious condition that affects many people. In Europe alone, it’s responsible for about half of all heart-related deaths and one in five natural deaths. The condition can come on very quickly, with little warning.
Some people might experience chest pain, shortness of breath, or nausea before the heart stops. Once it does, the person often loses consciousness and stops breathing normally. Without quick treatment, usually with CPR or a defibrillator, the person can die within minutes.
In the study, researchers wanted to see if there was a connection between sudden cardiac arrest and two drugs commonly used to treat high blood pressure and chest pain: nifedipine and amlodipine.
These drugs have been used for many years, and millions of people around the world take them to help manage their blood pressure and prevent chest pain.
The researchers looked at data from 2,503 patients who had experienced sudden cardiac arrest and compared them with 10,543 healthy people from a large health registry in Amsterdam.
Their findings showed that people taking a high dose of nifedipine (60 mg per day) were more likely to experience sudden cardiac arrest than those not taking the drug. However, the other drug, amlodipine, did not show the same risk.
To be sure about their results, the researchers checked their findings with data from another large group in Denmark.
This second analysis, involving 8,101 patients and 40,505 healthy people, confirmed the initial results: high doses of nifedipine were linked to a higher risk of sudden heart stoppage.
This finding is unexpected because nifedipine and amlodipine have been used safely by many patients for a long time.
However, sudden cardiac arrest is a very difficult condition to study because it happens so quickly and is often fatal, leaving little time for research. Previous studies may have missed this connection because of these challenges.
The researchers believe that more studies are needed to confirm this link before any changes are made to how doctors prescribe nifedipine or how patients take it. They stress that patients should not stop taking their medication without first talking to their doctor.
Instead, doctors and patients should be aware of this potential risk and discuss whether it’s necessary to adjust the dosage or consider other treatment options.
This study highlights the importance of ongoing research, even for drugs that have been used for many years. As we learn more, it’s crucial to update our understanding and approach to treatment to ensure the best possible outcomes for patients.
While the findings are still new and need further investigation, they offer a valuable reminder that what we know about medications can evolve, and staying informed is key to managing health risks effectively.
In summary, the study suggests that a high dose of nifedipine, a common drug for high blood pressure, may increase the risk of sudden heart stoppage.
This surprising discovery underscores the need for careful use of the drug and further research to fully understand the risks. For now, doctors and patients should have open conversations about the best way to manage high blood pressure while considering this new information.
If you care about blood pressure, please read studies about how diets could help lower high blood pressure, and 3 grams of omega-3s a day keep high blood pressure at bay.
For more information about blood pressure, please see recent studies that beetroot juice could help reduce blood pressure, and results showing cinnamon could help lower high blood pressure.
Copyright © 2024 Knowridge Science Report. All rights reserved.



