At the Massachusetts Institute of Technology (MIT), scientists are paving the way for a medical revolution.
They’ve developed a new method to 3D print tiny machines, called microfluidic devices, that can heat themselves.
This breakthrough could someday help in detecting diseases quickly, accurately, and affordably, even in remote parts of the world.
So, what are these microfluidic devices? They are miniature machines that control and manipulate tiny amounts of liquids, making them crucial for chemical reactions and disease detection. Think of the at-home COVID-19 test kits; they use a basic type of microfluidic device.
Traditionally, making these devices, especially the ones requiring specific temperatures for chemical reactions, has been complex and expensive. They are usually made in special clean rooms and involve costly materials like gold or platinum. But the MIT team has changed the game by using 3D printing to create these devices cheaply and efficiently.
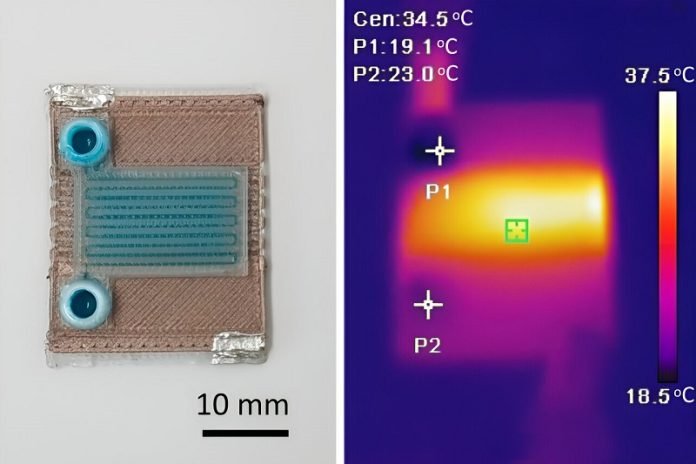
Using a method called multimaterial extrusion 3D printing, the researchers can print different materials through multiple nozzles, layer by layer, to build a complete device in one go. They use two types of materials: a common biodegradable plastic (PLA) and a modified version of PLA with copper nanoparticles.
This mixture turns the insulating PLA into an electrical conductor. When an electrical current passes through it, it heats up, thus heating the fluids in the device.
This innovative technique is not just cost-effective, requiring about $2 of materials, but also customizable. Engineers can design devices to heat fluids to specific temperatures or patterns, making them versatile for various applications.
Plus, these devices are small, about the size of a U.S. quarter, and can be produced quickly.
One of the most exciting aspects is that this technology could be a game-changer for disease detection in developing countries. These regions often lack access to expensive lab equipment, but with this new method, they could have an affordable solution.
However, there are some challenges to tackle. For instance, PLA can only withstand temperatures up to about 50°C, limiting its use for some chemical reactions that require higher temperatures. Also, to control the temperature precisely, the researchers need to integrate a third material that can sense temperature.
Looking ahead, the team is exploring ways to print magnets into these devices, which could sort or align particles for certain chemical reactions. They are also studying why PLA becomes conductive with certain impurities, as understanding this could enhance the devices’ capabilities.
This work isn’t just about the technology; it’s about simplicity and functionality. Norihisa Miki, a professor at Keio University in Tokyo, and Niclas Roxhed from Sweden’s KTH Royal Institute of Technology, both not part of this study, admire the simplicity and potential applications of this approach.
They see possibilities in biological sample processing and even implantable devices that dissolve over time.
In conclusion, MIT’s innovative 3D printing technique for self-heating microfluidic devices represents a significant step forward in medical technology.
Its simplicity, cost-effectiveness, and potential for widespread application could transform how we detect and diagnose diseases, making advanced medical technology more accessible worldwide.



