Atrial fibrillation—a form of irregular heartbeat, or arrhythmia—leads to more than 454,000 hospitalizations and nearly 160,000 deaths in the United States each year.
Globally, it is estimated that approximately 60 million people are affected by the condition.
In a study from the University of Arizona, scientists developed a battery-free, light-powered pacemaker that may improve the quality of life for heart disease patients.
Pacemakers are lifesaving devices that regulate the heartbeats of people with chronic heart diseases like atrial fibrillation and other forms of arrhythmia.
However, pacemaker implantation is an invasive procedure, and the lifesaving pacing the devices provide can be extremely painful. Additionally, pacemakers can only be used to treat a few specific types of disease.
In the study, the team developed a wireless, battery-free pacemaker that could be implanted with a less invasive procedure than currently possible and would cause patients less pain.
Currently available pacemakers work by implanting one or two leads, or points of contact, into the heart with hooks or screws.
If the sensors on these leads detect a dangerous irregularity, they send an electrical shock through the heart to reset the beat.
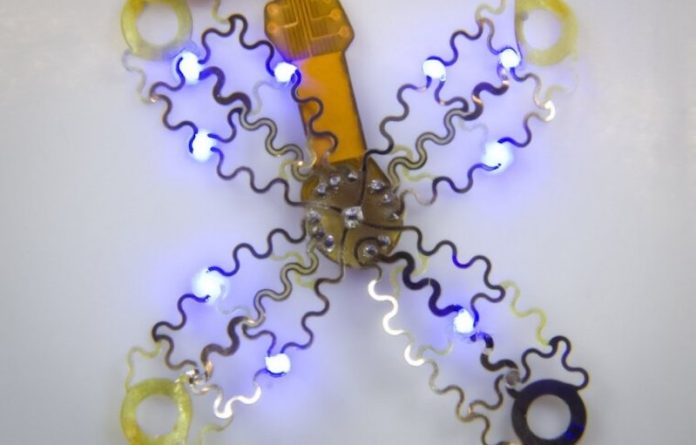
The new device would allow pacemakers to send much more targeted signals using a new digitally manufactured mesh design that encompasses the entire heart. The device uses light and a technique called optogenetics.
Optogenetics modifies cells, usually neurons, sensitive to light, then uses light to affect the behavior of those cells.
This technique only targets cardiomyocytes, the cells of the muscle that trigger a contraction and make up the beat of the heart.
This precision will not only reduce pain for pacemaker patients by bypassing the heart’s pain receptors, but it will also allow the pacemaker to respond to different kinds of irregularities in more appropriate ways.
For example, during atrial fibrillation, the upper and lower chambers of the heart beat asynchronously, and a pacemaker’s role is to get the two parts back in line.
To ensure the light signals can reach many different parts of the heart, the team created a design that involves encompassing the organ, rather than implanting leads that provide limited points of contact.
While the current version of the device has been successfully demonstrated in animal models, the researchers look forward to furthering their work, which could improve the quality of life for millions of people.
If you care about heart disease, please read studies about chronic itch linked to heart disease, and the best time to take vitamins to prevent heart disease
For more information about heart health, please see recent studies about how magnesium helps protect your heart rhythm, and results showing people who have the lowest heart disease and stroke risks.
The study was conducted by Philipp Gutruf et al and published in Science Advances.
Copyright © 2022 Knowridge Science Report. All rights reserved.



