Scientists from Washington University in St. Louis found that women who get recurrent urinary tract infections may be caught in a vicious cycle in which antibiotics given to eradicate one infection predispose them to develop another.
They found that a round of antibiotics eliminates disease-causing bacteria from the bladder but not from the intestines.
Surviving bacteria in the gut can multiply and spread to the bladder again, causing another UTI.
The research is published in Nature Microbiology and was conducted by Scott J. Hultgren et al.
One of the greatest frustrations regarding UTIs is that they so often recur. UTIs are caused by bacteria in the urinary tract and are characterized by frequent and painful urination.
A round of antibiotics usually clears up the symptoms, but the relief is often temporary: A quarter of women go on to develop a second UTI within six months.
Some unfortunate individuals get UTIs over and over and require antibiotics every few months.
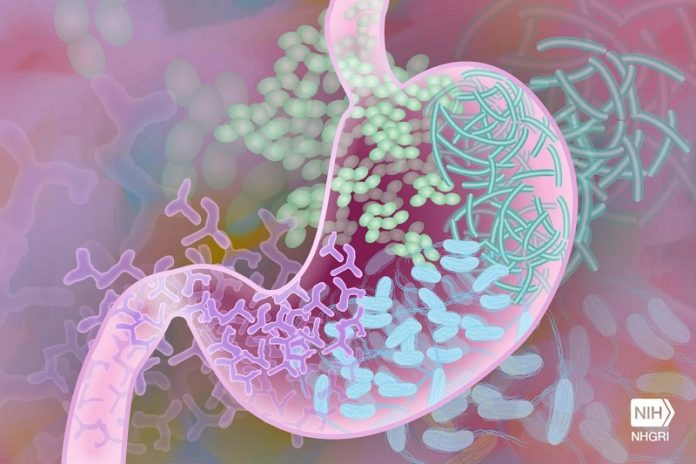
At the same time, repeated cycles of antibiotics wreak havoc on the community of helpful bacteria that normally live in the intestines, the so-called gut microbiome.
In the study, the researchers studied 15 women with histories of recurrent UTIs and 16 women without. All participants provided urine and blood samples at the start of the study and monthly stool samples.
Over the course of a year, 24 UTIs occurred, all in participants with histories of repeated UTIs. When participants were diagnosed with a UTI, the team took additional urine, blood, and stool samples.
The team found that similar to other disorders in which gut microbes and the immune system are linked, women with recurrent UTIs had less diverse microbiomes that were deficient in an important group of bacteria that helps regulate inflammation, and a distinct immunological signature in their blood indicative of inflammation.
The difference between the women who got repeated UTIs and those who didn’t, surprisingly, didn’t come down to the kind of E. coli in their intestines or even the presence of E. coli in their bladders.
Both groups carried E. coli strains in their guts capable of causing UTIs, and such strains occasionally spread to their bladders.
The real difference was in the makeup of their gut microbiomes. Patients with repeat infections showed decreased diversity of healthy gut microbial species, which could provide more opportunities for disease-causing species to gain a foothold and multiply.
Notably, the microbiomes of women with recurrent UTIs were particularly scarce in bacteria that produce butyrate, a short-chain fatty acid with anti-inflammatory effects.
The team says that women in the control group were able to clear the bacteria from their bladders before they caused disease, and women with recurrent UTI were not, because of a distinct immune response to bacterial invasion of the bladder potentially mediated by the gut microbiome.
The findings highlight the importance of finding alternatives to antibiotics for treating UTIs.
If you care about inflammation, please read studies about the cause of inflammation and clotting in severe COVID-19, and how avocados can help reduce inflammation.
For more information about inflammation, please see recent studies about hormone that could help reduce irregular heartbeat, inflammation, and results showing this drug for inflammation could help stop cancer metastasis.
Copyright © 2022 Knowridge Science Report. All rights reserved.



