Maureen Jenkins knew what was happening last October on a drive home from the cider mill with her husband, Jack, behind the wheel and two grandkids in the backseat.
Jack was having a stroke. The fact that she recognized the symptoms may have saved their lives.
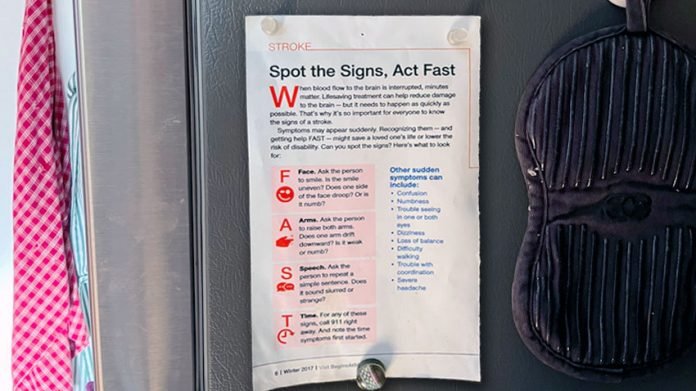
Jenkins attributes his wife’s quick thinking in part to a card displayed for years on the family’s refrigerator. The card spells out the word FAST, referring to stroke warning signs:
Face drooping, Arm going weak or numb, slurred Speech, Time to call 911 — a critical factor in a person’s outcome.
“My wife realized I wasn’t driving right,” said Jenkins, who experienced a sudden onset of right arm weakness, drooping face and slurred speech.
“She asked me to park the car and saw that the right side of my face was drooping. When she had me get out of the car and gave me the FAST test, she realized we needed to get to the hospital right away.
“I was very lucky that Maureen knew what was going on with me. And I was lucky to be near the University of Michigan when my stroke happened,” said the Ann Arbor, Michigan, resident.
Making the diagnosis
With his symptoms resolving upon arrival at the University of Michigan Health Emergency Department, Jenkins was first diagnosed with a TIA, or transient ischemic attack, sometimes referred to as a mini stroke.
A TIA happens when there is a temporary lack of blood flow to parts of the brain.
A TIA does not cause permanent damage and typically resolves on its own, which seemed to be the case for Jenkins.
While in the Emergency Department, however, his stroke symptoms returned, and he was treated with tissue plasminogen activator (tPA), a clot-busting medication administered intravenously (IV) within 4.5 hours of the first stroke symptoms.
“Once we determine a patient is having a stroke and eligible for treatment, standard of care is to administer IV tPA as soon as possible.
Immediate diagnosis and treatment is important as every second counts with a stroke,” said Cemal Sozener, M.D., co-director of the University of Michigan Health Comprehensive Stroke Center.
“The earlier this treatment can be delivered, the better the chances of reducing the long-term effects of stroke.”
When Jenkins’ symptoms began to worsen, with now left-sided weakness, left facial droop, difficulty speaking and vision issues, brain imaging confirmed the 75-year-old was having a basilar stroke.
This type of life-threatening stroke happens when a blockage occurs in the basilar artery, which serves as the main blood supply to the back of the brain.
A basilar stroke is a rare type of ischemic stroke, which, left untreated, has a mortality of nearly 90% and a very small chance for returning to independent living, says Sozener.
Risk factors for all types of stroke include:
High blood pressure. Untreated hypertension can cause blockage and calcification in blood vessels, ultimately restricting blood flow to the brain and resulting in stroke.
Heart disease. Carotid disease, a type of peripheral artery disease, causes narrowing of the arteries, which can restrict blood flow to the brain.
Atrial fibrillation (Afib), an irregular heart rhythm in which blood doesn’t flow smoothly, can result in a clot in the heart that can break free and travel to the brain.
Diabetes. Patients with diabetes are at an elevated risk for stroke due to the damaging effects of diabetes on the blood vessels.
Obesity, inactivity and diet. Excess body weight, lack of exercise and a poor diet can contribute to heart disease, high blood pressure and high cholesterol.
Age and gender. The risk of stroke goes up with age, with the vast majority of stroke patients over 50.
Ethnicity. Stroke is more common in Black and Hispanic populations.
Prior stroke/family history. Individuals who have suffered a stroke, or those with a sibling, parent or grandparent who has had a stroke, are at greater risk.
Experts in advanced therapies
The U-M Health Comprehensive Stroke Center neurointerventional team performed an endovascular thrombectomy to address Jenkins’ basilar artery blockage.
This minimally invasive procedure traps and removes the blood clot responsible for causing a stroke.
During the procedure, doctors thread a catheter through an artery in the groin or arm up to the blocked artery in the brain. A stent retriever is then inserted through the catheter to trap and remove the clot.
The complex procedure was successful, resulting in complete restoration of blood flow to the area of the brain supplied by the basilar artery, says Sozener.
“When a nurse showed me my scan and blood vessels, it was unbelievable to me that they could access a tiny blood vessel, grab the clot and pull it out of there,” said Jenkins, who credits the U-M Comprehensive Stroke Center team for quick action leading to his positive outcome.
“Mrs. Jenkins consented to her husband’s inclusion in this national research study being performed at U-M,” said Sozener, noting:
“The goal of the study is to use medications to keep the affected blood vessel open and prevent the artery from reoccluding following IV tPA in an attempt to improve long-term stoke outcomes.
“Mr. Jenkins did exceptionally well and was able to be discharged home within three days of his stroke, which is the type that, sadly, kills many people in the U.S. each year,” said Sozener.
A successful outcome
“Following the thrombectomy, I wore a heart monitor for two weeks to see if I had atrial fibrillation, a heart rhythm condition that can lead to stroke,” said Jenkins, whose risk factors included hypertension and a TIA, which he experienced 15 years earlier.
“A prior TIA is a strong risk factor for suffering a subsequent stroke. It’s your body’s way of telling you something is wrong,” said Sozener.
Because Jenkins was not diagnosed with Afib, he’s able to take a low-dose aspirin instead of a more aggressive blood thinner.
“I had an at-home nurse checking in on me and did physical therapy to make sure I didn’t have any balance issues,” said Jenkins, who was also concerned about stroke-related speech or cognitive issues.
To ease his mind, he saw a speech and cognitive therapist who determined there were no signs of impairment, other than slight memory issues attributed to the normal aging process.
Now seven months after his stroke, Jenkins is feeling more at ease. “I know if you’ve had a stroke, you’re more likely to have another one, so I was worried about it for a while. It was like an unwanted guest in my home,” he said.
Jenkins works each day to stay sharp with brain-stimulating activities like the New York Times crossword puzzle and enjoys spending time with his grandchildren as well as other family members and friends. He also is an avid reader and walker.
“I try to walk four miles three days a week at a quick pace to get my heart rate up. This gives me the recommended 150 minutes per week of cardiac exercise.”
Jenkins says the stroke has affected his outlook, resulting in a combination of worry (which is subsiding) and motivation to do more worthwhile things in his life.
“I feel perfectly normal now and completely lucky,” he said, noting his appreciation for the quick action of his wife and the expertise of the U-M Health Comprehensive Stroke Center team.
Act FAST
Sozener reinforces his message to anyone who may think they’re having a stroke.
“If you think you or a loved one is having a stroke, call 911 immediately to take you to the nearest emergency department,” said Sozener.
“Doctors are able to communicate with the EMS team to understand your condition and to prepare for your arrival.”
Quick thinking is imperative, he says.
“Every minute counts when you’re having a stroke. The lack of blood flow to the brain means the greater the chances of permanent damage.
We want to restore blood flow as soon as possible. There is a narrow time window to achieve a good outcome,” said Sozener.
Written by Jane Racey Gleeson.
If you care about stroke, please read studies about how to prevent heart attack and stroke, and drinking coffee this way may prevent heart disease, stroke.
For more information about stroke, please see recent studies about new way to prevent recurrent stroke, and results showing this blood thinner drug plus aspirin could strongly reduce stroke risk.



