One of the most vexing aspects of the COVID-19 pandemic is doctors’ inability to predict which newly hospitalized patients will go on to develop severe disease.
In a new study, researchers found that a relatively simple and rapid blood test can predict—within a day of a hospital admission—which patients with COVID-19 are at the highest risk of severe complications or death.
The research was conducted by scientists at Washington University School of Medicine in St. Louis
In the study, the team evaluated 97 patients with COVID-19, measuring their mitochondrial DNA levels on the first day of their hospital stays.
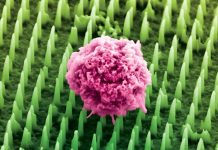
The blood test measures levels of mitochondrial DNA, a unique type of DNA molecule that normally resides inside the energy factories of cells.
Mitochondrial DNA spilling out of cells and into the bloodstream is a sign that a particular type of violent cell death is taking place in the body.
The team found that mitochondrial DNA levels were much higher in patients who eventually were admitted to the ICU, intubated, or died.
They found this association held independently of a patient’s age, sex, and underlying health conditions.
Further, the test predicted outcomes as well as or better than existing markers of inflammation currently measured in patients hospitalized with COVID-19.
Most other markers of inflammation measured in patients with COVID-19, including those still under investigation, are general markers of systemic inflammation, rather than inflammation specific to cell death.
The researchers said the test could serve as a way to predict disease severity as well as a tool to better design clinical trials, identifying patients who might, for example, benefit from specific investigational treatments.
They also said they would like to evaluate whether the test could serve as a way to monitor the effectiveness of new therapies. Presumably, effective treatments would lower mitochondrial DNA levels.
One author of the study is Andrew E. Gelman, Ph.D.
The study is published in JCI Insight.
Copyright © 2021 Knowridge Science Report. All rights reserved.