People infected with COVID-19 experience a wide range of symptoms and severities, the most commonly reported including high fevers and respiratory problems.
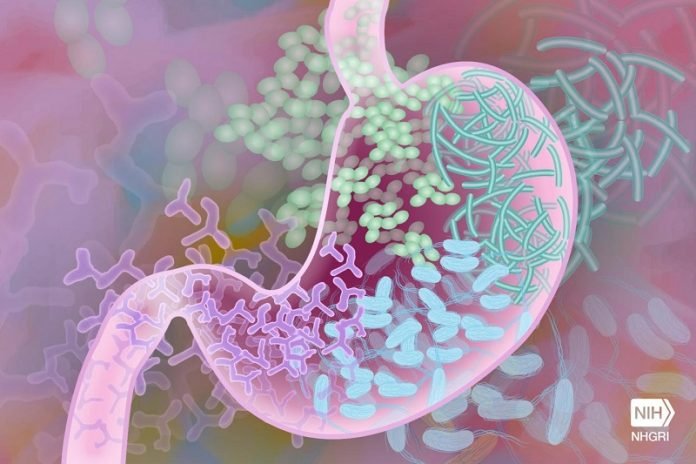
However, autopsy and other studies have also revealed that the infection can affect the liver, kidney, heart, spleen—and even the gastrointestinal tract.
Many patients hospitalized with breathing problems also have diarrhea, nausea and vomiting, suggesting that when the virus does get involved in the GI tract it increases the severity of the disease.
In a new study, researchers examined emerging evidence suggesting that poor gut health adversely affects COVID-19 prognosis.
They proposed that gut dysfunction—and its associated leaky gut—may exacerbate the severity of infection by enabling the virus to access the surface of the digestive tract and internal organs.
These organs are vulnerable to infection because they have widespread ACE2—a protein target of SARS-CoV-2—on the surface.
The research was conducted by a team from Korea University.
Studies have demonstrated that people with underlying medical conditions including high blood pressure, diabetes, and obesity face a higher risk of severe COVID-19.
Risk also increases with age, with older adults most vulnerable to the most serious complications and the likelihood of hospitalization.
But both of these factors—advanced age and chronic conditions—have a well-known association with altered gut microbiota.
This imbalance can affect gut barrier integrity, Kim noted, which can allow pathogens and pathobionts easier access to cells in the intestinal lining.
In the study, the team found recent studies showed reduced bacterial diversity in gut samples collected from COVID-19 patients, compared to samples from healthy people.
The disease has also been linked to a depletion of beneficial bacterial species—and the enrichment of pathogenic ones.
A similar imbalance has been linked to influenza A infection, though the 2 viruses differ in how they change the overall microbial composition.
The depleted bacterial species associated with COVID-19 infection include some families that are responsible for producing butyrate, a short-chain fatty acid, which plays a pivotal role in gut health by reinforcing gut-barrier function.
The team found that wealthy countries with good medical infrastructure—including the United States and nations in Western Europe—were among the hardest hit by the virus.
The “western diet” that’s common in these countries is low in fiber, and a fiber-deficient diet is one of the main causes of altered gut microbiomes. Such gut microbiome dysbiosis leads to chronic diseases.
The pathogenesis of COVID-19 is still not fully understood.
The team says if future studies do show that gut health affects COVID-19 prognosis, then clinicians and researchers should exploit that connection for better strategies aimed at preventing and managing the disease.
Eating more fiber may lower a person’s risk of serious disease. And fecal microbiota transplantation might be a treatment worth considering for patients with the worst cases of COVID-19.
One author of the study is microbiologist Heenam Stanley Kim, Ph.D.
The study is published in mBio.
Copyright © 2021 Knowridge Science Report. All rights reserved.



