In a new study, researchers found examined six patients with brain damage caused by COVID-19 using a specialized magnetic resonance (MR) technique.
They found that these patients with neurological symptoms show some of the same metabolic disturbances in the brain as other patients who have suffered oxygen deprivation (hypoxia) from other causes
The research was conducted by a team at Massachusetts General Hospital (MGH).
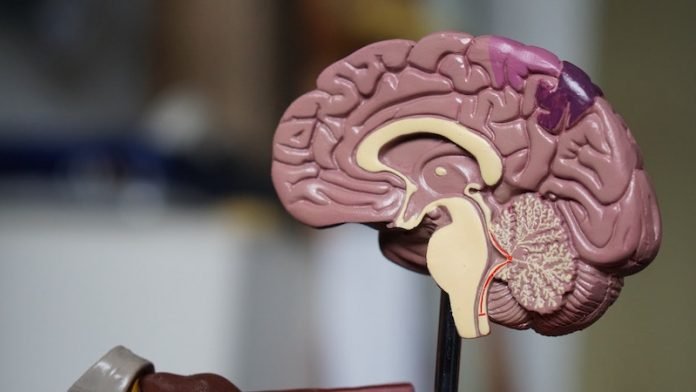
While it is primarily a respiratory disease, COVID-19 infection affects other organs, including the brain.
It is thought that the disease’s primary effect on the brain is through hypoxia, but few studies have examined the specific types of damage that distinguish COVID-19-related brain injury.
Several thousand patients with COVID-19 have been seen at the MGH since the outbreak began early this year, and this study included findings from three of those patients.
The severity of neurological symptoms varies, ranging from one of the most well-known—a temporary loss of smell—to more severe symptoms such as dizziness, confusion, seizures, and stroke.
The researchers used 3 Tesla Magnetic Resonance Spectroscopy (MRS), a specialized type of scanning that is sometimes called a virtual biopsy.
They found that COVID-19 patients’ brains showed N-acetyl-aspartate (NAA) reduction, choline elevation, and myo-inositol elevation, similar to what is seen in other patients with white matter abnormalities after hypoxia without COVID.
One of the patients with COVID-19 who showed the most severe white matter damage had strong lactate elevation on MRS, which is another sign of brain damage from oxygen deprivation.
Two of the three COVID-19 patients were in the intensive care unit at the time of imaging, which was conducted as part of their care.
One had COVID-19-associated white matter abnormalities. Another had experienced a recent cardiac arrest and showed subtle white matter changes on structural MR.
The third had no recent cardiac arrest. The non-COVID control cases included one patient with white matter damage due to hypoxia from other causes, one with sepsis-related white matter damage, and a normal, age-matched, healthy volunteer.
The team says future work needs to find whether it is just the decrease in oxygen to the brain that is causing these white matter changes or whether the virus is itself attacking the white matter.
They believe that compared to conventional structural MR imaging, MRS can better characterize pathological processes, such as neuronal injury, inflammation, demyelination, and hypoxia.
It could be used as a disease and therapy monitoring tool.
One author of the study is Eva-Maria Ratai, Ph.D.
The study is published in the American Journal of Neuroradiology.
Copyright © 2020 Knowridge Science Report. All rights reserved.



