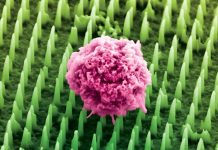
In a recent study at Oak Ridge National Laboratory, researchers analyzed the lung fluid cells from COVID-19 patients.
They used the nation’s fastest supercomputer to check gene expression patterns that may explain the runaway symptoms produced by the body’s response to SARS-CoV-2.
They found that genes related to one of the body’s systems responsible for lowering blood pressure—the bradykinin system—appear to be excessively “turned on” in the lung fluid cells of those with the virus.
Based on the analyses, the researchers say that bradykinin—the compound that dilates blood vessels and makes them permeable—is overproduced in the body of COVID-19 patients.
Related systems either contribute to overproduction or cannot slow the process. Excessive bradykinin leads to leaky blood vessels, allowing fluid to build up in the body’s soft tissues.
The study is published in eLife. One author is Dan Jacobson of the Department of Energy’s Oak Ridge National Laboratory.
Much attention has focused on what’s known as the cytokine storm, a severe reaction in which the body releases an excess of cytokines, a variety of small proteins that help regulate the immune system.
The team thinks a bradykinin storm may instead be to blame for much of the viral pathogenesis.
If the disease mechanism model is accurate and substantiated by experimental analysis, it may mean that existing medicines could be repurposed to slow the pathogenesis of COVID-19.
This would require extensive clinical trials of drugs currently used to treat other bradykinin-related conditions.
The bradykinin storm could explain the wide variety of symptoms experienced by COVID-19 patients, such as muscle pain, fatigue, nausea, vomiting, diarrhea, headaches, and decreased cognitive function.
Similar symptoms are also experienced by patients with other bradykinin-related conditions such as hereditary angioedema, a genetic condition that is characterized by episodes of severe swelling throughout the body.
In the study, the team compared the genes of 9 COVID-19 patients against a control group and analyzed population-scale gene expression data—17,000 samples from uninfected individuals—to see which genes were normally co-expressed, or turned on or off at the same time.
They found an increased expression of enzymes that can trigger the production of bradykinin and a decreased expression of enzymes that would break down bradykinin—the perfect storm.
The team also uncovered that an enzyme that forestalls the bradykinin cascade—the angiotensin-converting enzyme, known as ACE—was less expressed in COVID-19 patients.
At least ten existing drugs are known to act on the specific pathways the team studied, but large-scale clinical trials are needed to determine whether they might be effective at treating COVID-19.
The lungs of COVID-19 patients are known to have an increased amount of hyaluronic acid, a gooey substance found in connective tissues that can trap around 1,000 times its own weight in water to form a hydrogel.
The team also found that genes in the cells of COVID-19 patients increased the production of the substance and decreased its breakdown.
The findings suggest that further experimental study of drug compounds known to slow the synthesis of hyaluronic acid and the mechanisms involved in the process is warranted.
Copyright © 2020 Knowridge Science Report. All rights reserved.