Ever since SARS-CoV-2 first appeared, researchers have been trying to understand whether sometimes the immune system does more harm than good during the acute phase of COVID-19.
In a new study, researchers found that a multi-layered, virus-specific immune response is important for controlling the virus during the acute phase of the infection and reducing COVID-19 disease severity.
The findings point to a much bigger role for T cells than antibodies. A weak or uncoordinated immune response, on the other hand, predicts a poor disease outcome.
The study suggests that vaccine candidates should aim to elicit a broad immune response that includes antibodies, helper and killer T cells to ensure protective immunity.
The findings could also explain why older COVID-19 patients are much more vulnerable to the disease.
With increasing age, the reservoir of T cells that can be activated against a specific virus declines, and the body’s immune response becomes less coordinated, which looks to be one factor making older people drastically more susceptible to severe or fatal COVID-19.
The research was conducted by a team at La Jolla Institute for Immunology.
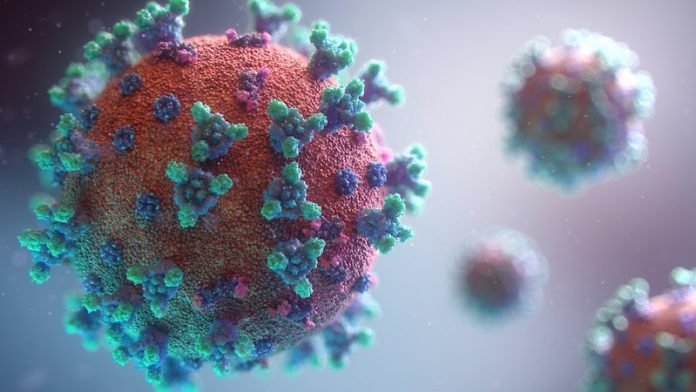
When SARS-CoV-2 (or any other virus) infiltrates the body, the innate immune system is first on the scene and launches a broad and unspecific attack against the intruder.
It releases waves of signaling molecules that incite inflammation and alert the immune system’s precision forces to the presence of a pathogen.
Within days, the so-called adaptive immune system tools up and moves with pinpoint precision against the virus, intercepting viral particles and killing infected cells.
The adaptive immune system consists of three branches: antibodies; helper T cells (Th), which assist B cell to make protective antibodies; and killer T cells (CTL), which seek out virus-infected cells and eliminate them.
In the study, the team collected blood samples from 50 COVID-19 patients and analyzed all three branches of the adaptive immune system—SARS-CoV-2 specific antibodies, helper and killer T cells—in great detail.
What the team found was that similar to their previous study all fully recovered individuals had measurable antibody, helper and killer T cell responses, while the adaptive immune response in acute COVID-19 patients varied more widely with some lacking neutralizing antibodies, others helper or killer T cells or any combination thereof.
The effect was magnified when the researchers broke down the dataset by age.
People over the age of 65 were much more likely to have poor T cell responses and a poorly coordinated immune response, and thus have much more severe or fatal COVID-19.
Thus, part of the massive susceptibility of the elderly to COVID-19 appears to be a weak adaptive immune response, which may be because of fewer naïve T cells in the elderly.
In line with what other research teams had found before, antibodies don’t seem to play an important role in controlling acute COVID-19.
Instead, T cells and helper T cells in particular are linked to protective immune responses.
The team says if vaccination is successful, vaccine-induced antibodies are ready to intercept the virus when it shows up at the doorstep.
In contrast, in a normal infection, the virus gets a head start because the immune system has never seen anything like it.
By the time the adaptive immune system is ready to go during primary infection, the virus has already replicated inside cells and antibodies can’t get to it.
One author of the study is Shane Crotty, Ph.D.
The study is published in Cell.
Copyright © 2020 Knowridge Science Report. All rights reserved.



