Iron is an essential mineral that we get from food or from supplements, which helps the body to make the red blood cells that carry oxygen around our bodies.
Iron absorption is tightly regulated at the whole body, organ, and cell levels to keep our iron stores balanced and maintain health. When too much iron is absorbed by cells it can lead to a build-up of iron within the cells.
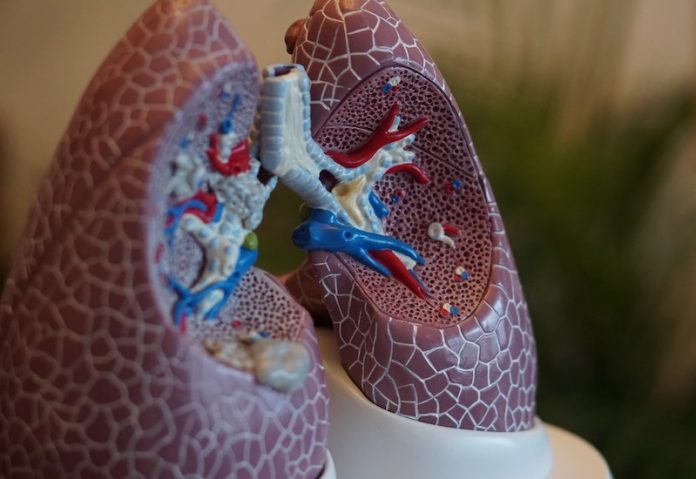
In a recent study from the University of Newcastle and elsewhere, researchers found that iron build-up in the lung cells and tissues is linked to worse asthma symptoms and lower lung function.
The study includes data from asthma patient samples and mouse models and is the first to definitively show a relationship between iron build-up in the lung cells and tissues and the severity of asthma.
The researchers also showed that iron build-up in the lungs triggers immune system responses that are typical in asthma and lead to worsening of the disease.
This includes effects like increased mucus secretion and scarring of the lungs, which result in the narrowing of the airways and making breathing difficult.
The study is published in the European Respiratory Journal. The lead author is Jay Horvat, Associate Professor of Immunology and Microbiology.
In the study, the researchers used a combination of asthma patient samples and experimental models to test irregular iron absorption into lung cells and to assess how lung cell iron levels affect disease severity.
First, the researchers examined airway cell iron levels in 11 severe and 12 mild-to-moderate asthma patients and compared their iron levels with 12 healthy people who did not have asthma.
Asthma severity was determined by how much air a person could breathe out in one second and based on the frequency of experiencing asthma symptoms.
The researchers found that iron levels outside of the lung cells were lower in asthma patients compared with healthy people; iron levels were also much lower in severe asthmatics compared with mild-to-moderate asthmatics.
In contrast, iron levels within the lung cells were markedly higher in the bronchoscope ‘wash’ samples of mild-to-moderate and severe asthmatics compared with healthy people.
The difference in lung cell iron levels between severe asthmatics compared with mild-to-moderate asthmatics was not significant, but having high levels of iron in the lung cells and less iron outside of cells was linked to more severe airflow obstruction.
Taken together, the results show that lower iron levels outside of cells and higher iron levels within cells were both linked to lower lung function and worsen asthma.
Next, the researchers carried out lab tests using two different mouse models to examine the effects of increasing lung cell iron levels on asthma severity.
They found that increasing the lung cell iron levels caused inflammatory cell responses such as increased mucus secretion and scarring in the airways, which leads to worsening of asthma.
The researchers say the findings offer great potential for the development of asthma treatments that target irregular iron absorption in the lung cells and tissues.
But more research is needed to determine why there is increased absorption in the lungs of asthmatics.
The research team is now examining ways to modify the iron storage process in lung cells, and whether it is possible to alter the number of the cells that are responsible for iron absorption into the lung cells.
They hope to develop these approaches into therapies for not only asthma but also for rare lung diseases like idiopathic pulmonary fibrosis.
Copyright © 2020 Knowridge Science Report. All rights reserved.



