In a new study, researchers have discovered a deficiency in the brains of people with schizophrenia that could lead to the development of new drug therapies.
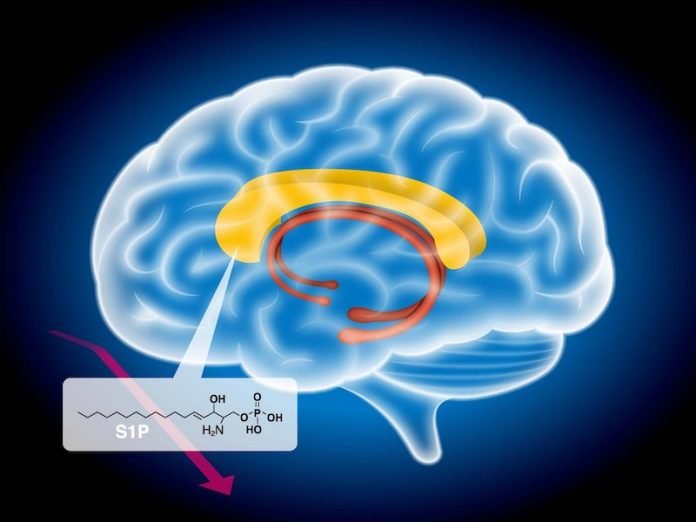
They found that schizophrenia was linked to lower than normal levels of S1P, a type of fatty molecule found in the white matter of the brain.
Preventing S1P degradation might, therefore, be a new direction for drug development in treating schizophrenia.
The research was conducted by a team at the RIKEN Center for Brain Science (CBS) in Japan.
Although schizophrenia is a well-known mental disorder that affects the brain, how it does so remains somewhat of a mystery.
Scientists have known for some time that the brains of people with schizophrenia have less white matter than normal brains.
White matter in the brain is made from oligodendrocytes, special cells that wrap around the parts of neurons that carry outgoing signals, which helps them communicate with each other.
Characteristic symptoms of schizophrenia include hallucinations and the inability to distinguish reality from fantasy, which might originate in white matter abnormalities that cause irregular communication between neurons.
In recent years, drug therapy for schizophrenia has come to a stand-still. Most of the drugs available for schizophrenia are based on dopamine, but they are ineffective in about one out of every three patients.
In the study, the team examined sphingolipids, a group of lipids known to have many functions, some related to white matter.
Postmortem analysis of the large white matter tract that connects the left and right sides of the brain showed a severe deficiency in S1P, a sphingolipid necessary for oligodendrocyte production.
Further tests showed that although normal amounts of S1P had been produced, it was metabolized and degraded when it should not have been.
The team says drugs that prevent S1P degradation could be particularly effective in treating schizophrenia.
This was the first psychiatric study of the postmortem brain to use mass spectroscopic analysis, and the discovery would not have been possible without the newly established comprehensive technique for screening sphingolipids.
After finding S1P sphingolipid deficiency in schizophrenia, the researchers examined the postmortem brains of people with bipolar disorder or major depressive disorder.
They found that S1P levels did not differ from what they found in normal brains, indicating that the problem is specific for schizophrenia and not a common feature of mental disorders.
The lead author of the study is Takeo Yoshikawa, a team leader at RIKEN CBS.
The study is published in Schizophrenia Bulletin.
Copyright © 2020 Knowridge Science Report. All rights reserved.



