In 2013, nearly 3 million men in the U.S. were battling prostate cancer, a serious disease that affects the prostate, a small gland that produces seminal fluid in men.
According to the National Cancer Institute, more than 180,000 new cases were expected in 2016, and over 26,000 men were likely to lose their lives to the disease.
But there’s good news on the horizon! Scientists have made a breakthrough in finding a way to detect the spread of prostate cancer throughout the body, even in hard-to-reach places.
This research was published in The Journal of Nuclear Medicine’s December issue and focused on a new imaging agent called Zr-89-desferrioxamine-IAB2M (we’ll call it Zr-89-Df-IAB2M, for short).
This agent is a type of mini-antibody that targets a specific marker present in prostate cancer cells called PSMA.
Dr. Neeta Pandit-Taskar from the Memorial Sloan Kettering Cancer Center in New York City explains, “This new agent works faster than previous methods due to its small size and is safe for patients.”
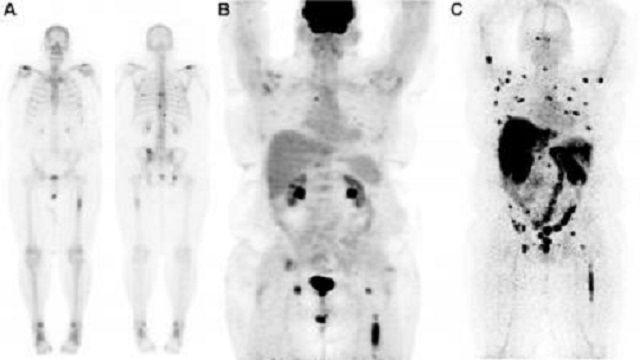
The way it works is pretty cool: the minibody attaches itself to prostate cancer cells anywhere in the body. When attached, it emits particles that can be detected by a type of scanner called a PET (positron emission tomography) scanner. The result is a scan that shows ‘hot spots’ where the cancer has spread.
Dr. Pandit-Taskar continues, “This new method even allows us to see cancer cells that have spread to the bone, which was notoriously tough to do with older methods.”
To test this new method, the scientists used 18 patients and compared the new method with older imaging techniques like CT scans, MRIs, and traditional PET scans.
When using the new agent, the scientists found that scans were positive in 17 out of the 18 patients, meaning it successfully detected the spread of the cancer in these cases. Interestingly, it found cancer in places that older methods couldn’t, thus proving to be more effective.
“Scanning with this new Zr-89 radiolabeled minibody allowed us to detect more locations of the disease in patients than with conventional scanning methods,” says Dr. Pandit-Taskar. She is hopeful that this new technology will help doctors make better and earlier decisions about a patient’s treatment.
In addition to improving detection, this new agent could be used to direct biopsies, making them more accurate. It might even be used in the future to directly target radiotherapy, a type of cancer treatment.
This new method is a massive step in the right direction for diagnosing and treating prostate cancer, and we are hopeful for what it means for the future of cancer treatments.



